 |
The decision on when to give a child their first pair of glasses might not be as clear-cut as the guidelines lead us to believe. The current guidelines from optometry and ophthalmology are set up based on age and refractive error. If a child is over a certain age and you measure a refractive error of roughly a set amount, the recommendation is that you prescribe that amount so that the child can have the best possible vision.
This sounds great in theory, but as we have discussed in this column time and time again, there is so much more to vision than seeing a 20/20-sized letter from a specified distance.
We must always take into account the visual needs of the child, which includes their development. The question at hand is whether all kids absolutely need to see 20/20. Yes, we said it out loud (well, wrote it). When we are prescribing, we must account for age, visual needs and development. For example, the visual needs of a child with a developmental disability are often different than those of a normally developing child. The visual needs of a three-year-old are quite different than those of an eight-year-old, and even more different than the needs of a 15-year-old.
Before we delve into a few case examples, two articles help to lay the groundwork for our thinking.
Langford and Hug studied the classroom visual demands of children from kindergarten to fifth grade. They measured vertical letter sizes at distance and near and the distances of the various desk rows. A near distance of 16 inches was assumed, but that itself might be too far away for some children in this age group, in our opinion. The authors found that from kindergarten to second grade the visual acuity demand at distance ranges from 20/100 to 20/300, and from grades three to five it approximates 20/60. At near, the demand for all grades ranged from 20/100 to 20/500. In their conclusions, the authors noted that “children with mild to moderate distance refractive errors may be able to perform in classroom activities without correction.”1 We will come back to this concept later.
 |
|
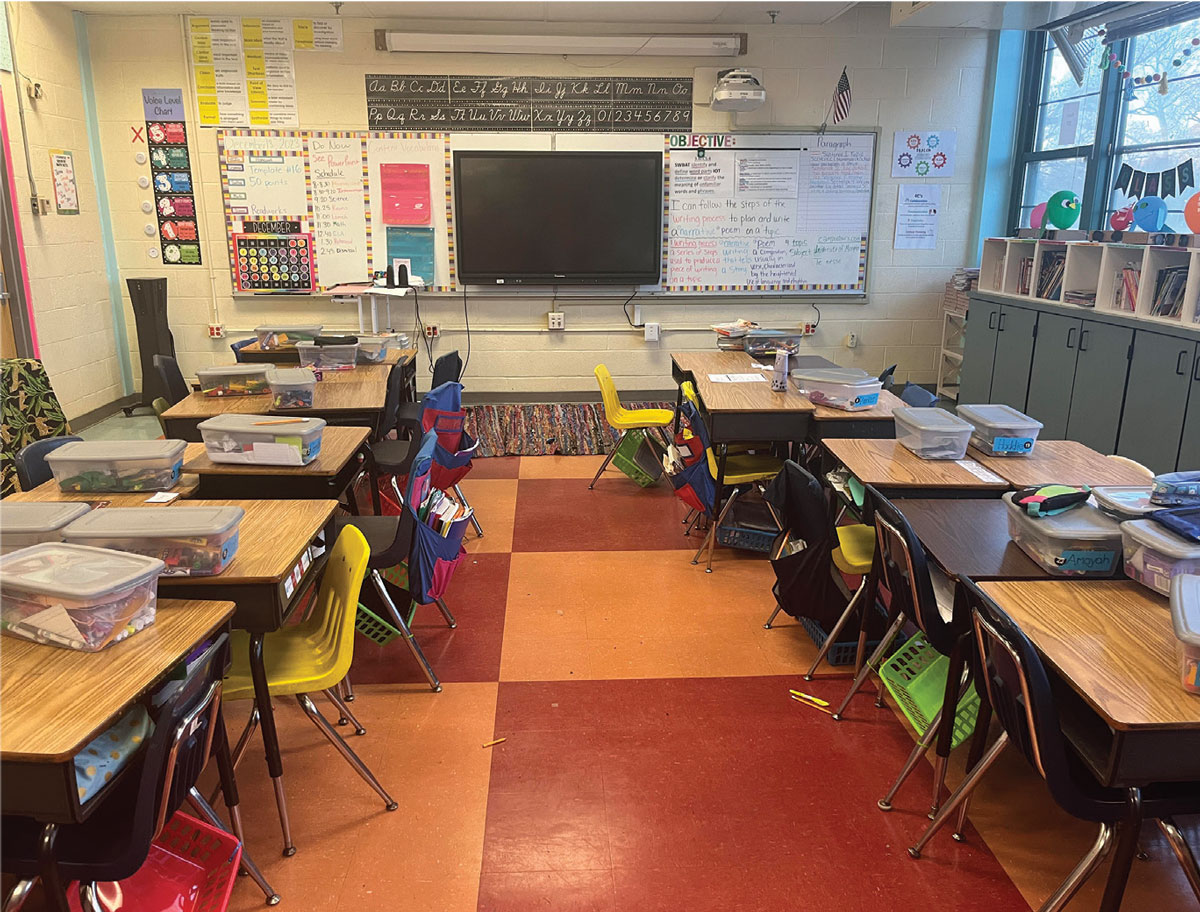
Fig. 1. Second grade classroom in a private school, where the farthest seating is only about 10 feet from the whiteboard. Click image to enlarge. |
Another study (by Negiloni et al.) looked at 33 classrooms from grades four to 12 in India. The minimum visual acuity demand at specific desks from the various grades was evaluated. The average distance and near threshold visual acuity demands were approximately 20/40 and 20/55, respectively. The mean visual acuity demand in grades four to eight was 20/45, and in grades nine to 12 it was 20/36.2 The authors point out that lighting, letter contrast and legibility can, of course, also play a role in and impact the visual demand. As we have both performed our share of vision screenings, we can attest that the lighting in classrooms can often be lacking or variable.
Once again, before we present a few cases, we need to look at a few classrooms that showcase some of the challenges in using a refractive error-based guideline. Figure 1 is from a local private school. You will notice that this second grade classroom is not set up in the traditional row design that many of us used when we were in school. The desks are instead arranged in a sort of semicircle, and even the set of desks farthest from the whiteboard is only about 10 feet away. The closest set of desks is only about three to four feet from the front.
Figure 2 shows a third grade classroom from a local public school. At once, you should notice a different desk configuration; none of the desks actually face the front of the room! The kids in this classroom must turn their heads and/or bodies to see what is written at the front of the classroom. Our necks hurt just thinking about it! The closest desks are about five to six feet away, and the farthest are about 12 to 13 feet from the front. The observation can be made here that even though the classrooms are quite different, there is ample opportunity to move a child to the front of the room if there is less than perfect vision. Now, on to the cases!
 |
|
Fig. 2. Third grade classroom at a public school. Note how close kids can be moved to accommodate visual need. Click image to enlarge. |
Case 1
A four-year-old presented for a routine examination without parental complaint of squinting or getting too close to the television. Development was normal: crawling, talking, walking and shape recognition occurred at the expected times. Visual acuity was 20/40 at distance and 20/40 at near OU. Near point of convergence was “to the nose” x3 and stereo showed gross global forms at 400 seconds of arc. Cover test was ortho at distance and three exophoria at near. Retinoscopy was plano -2.00x180 OD and OS.
To anticipate your question: Yes, this child will stand a good chance of needing glasses down the line, since with-the-rule cylinder of this power tends to be fairly consistent as children age. However, the question you should ask is whether the child needs this correction now. In our opinion and based on the Langford and Hug study, the child’s visual acuity meets their visual needs. We decided simply to sit back and watch for another year while also educating his parents accordingly.
Case 2
An eight-year-old presented for a routine examination without complaints of squinting or having trouble seeing the board in school. Development was normal and the child was performing well in school, with reading on grade level. Visual acuity was 20/30 at distance and 20/30 at near OU. Near point of convergence was “to the nose” x3 and stereo showed local forms at 25 seconds of arc. Cover test was ortho at distance and 4 exophoria at near. Accommodative amplitude was 14.00D OD and 15.00D OS. Retinoscopy was -0.75 -0.25x180 OD and OS.
Since there were no complaints from the child or parents, we decided against prescribing at the current time and suggested that the child be moved towards the front of their classroom. We did decide to educate the parents on myopia control, and both they and patient agreed to begin atropine 0.05% to reduce the expected myopic progression due to age and increased nearpoint demand. Based on the Negiloni study, the child’s 20/30 acuity is below the average visual threshold, and moving them up closer to the front would help even more.
Takeaways
While both of these cases highlight “need” according to refractive error, based on their histories—including normal development and lack of symptoms or complaints—we chose not to act. These decisions were purposeful and deliberate. Prescribing is the easy choice, but it is one that comes with potential consequences to visual development. We challenge you to consider the alternative option of temporarily withholding prescription, instead letting the child enjoy more time exploring their world free of glasses.
Dr. Taub is a professor and co-supervisor of the Vision Therapy and Pediatrics residency at Southern College of Optometry (SCO) in Memphis. He specializes in vision therapy, pediatrics and brain injury. Dr. Schnell is a professor at SCO and teaches courses on ocular motility and vision therapy. She works in the pediatric and vision therapy clinics and is co-supervisor of the Vision Therapy and Pediatrics residency. Her clinical interests include infant and toddler eye care, vision therapy, visual development and the treatment and management of special populations. They have no financial interests to disclose.
1. Langford A, Hug T. Visual demand in elementary school. J Pediatr Ophthalmol Strabismus. 2010;47(3):152-6. 2. Negiloni K, Ramani KK, Sudhir RR. Do school classrooms meet the visual requirements of children and recommended vision standards? PLoS One. 2017;12(4):e0174983. |

