OCT angiography (OCT-A) and an even more advanced imaging platform—adaptive optics scanning laser ophthalmoscopy—have shown much promise for detecting early structural changes in the retinal vasculature compared to conventional exam techniques. However, a recent study in Ophthalmology Science suggests a promising option for early detection and potential intervention for diabetic retinopathy (DR): retinal fluorescein videoangiography.
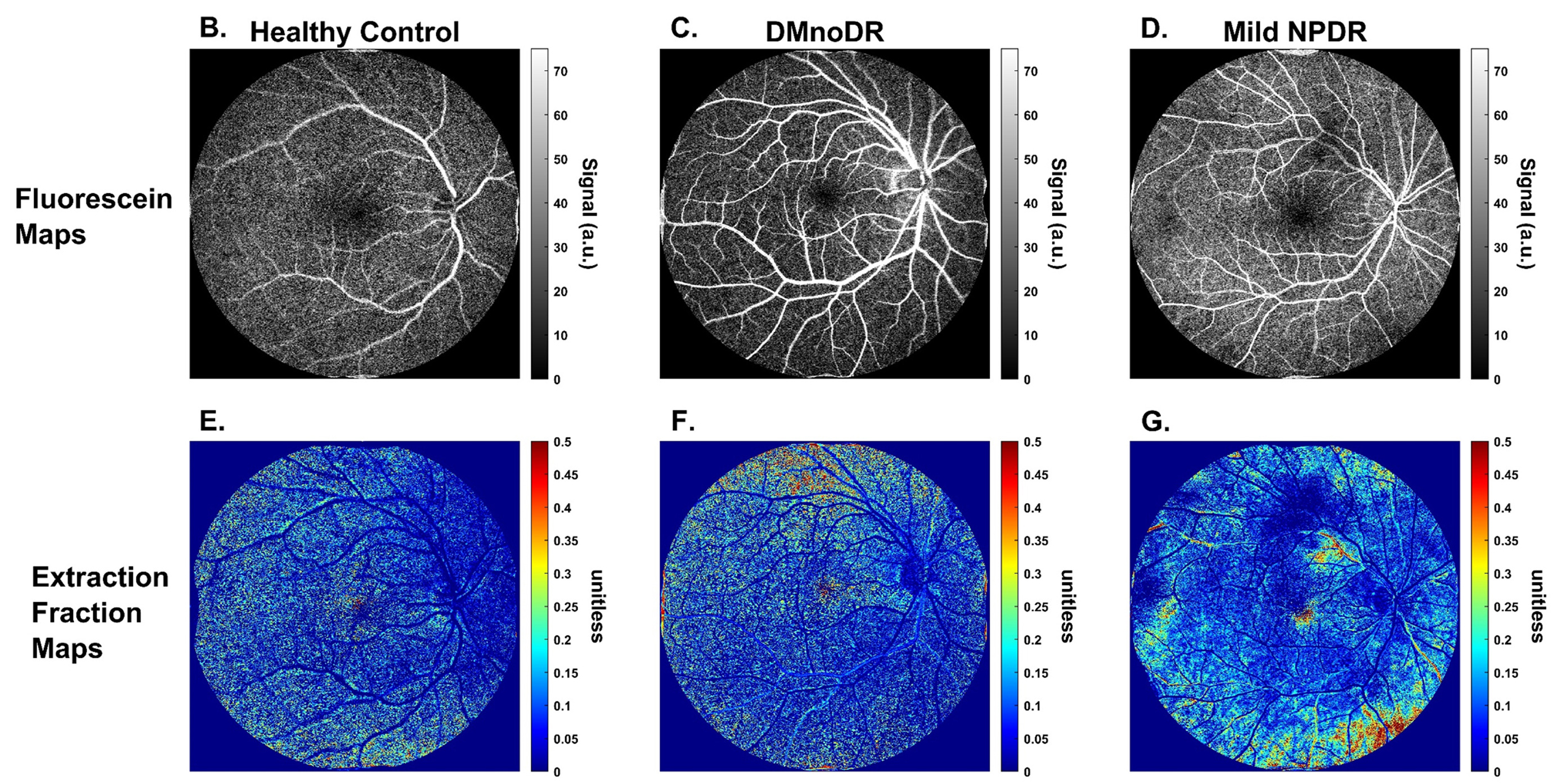 |
| A routine retinal fluorescein videoangiography dataset could be used to quantify vascular permeability—a functional parameter of the vasculature that is hypothesized to be affected prior to the early structural changes detectable by OCT-A and AO- and adaptive optics scanning laser ophthalmoscopy—in human retinas. These images from the study show examples of pixel-by-pixel fluorescein maps for (A) a control subject, (B) a diabetes subject with no DR, and (C) an individual with mild NPDR with corresponding extraction fraction maps (D, E, F) for each. Photo: Vavrek SR, et al. Ophthalmol Sci. October 25, 2024. Click image to enlarge. |
Researchers based in Chicago believe that retinal vascular permeability could be a possible biomarker for determining preclinical retinal pathology in patients with diabetes. In early results from a larger five-year clinical study, the researchers determined that measures of vascular permeability were significantly higher in patients with diabetes mellitus but with no signs of retinopathy compared to healthy controls.
The study included seven healthy controls, 22 patients with diabetes mellitus and no clinical signs of retinopathy and seven patients with mild nonproliferative diabetic retinopathy (NPDR). All participants underwent routine retinal fluorescein videoangiography. Each fluorescein videoangiography dataset was analyzed with a dynamic tracer to estimate several parameters related to blood flood and vascular permeability.
“Extraction fraction, i.e., the fluorescein dye leakage measured during one pass through surrounding retinal tissue, is extracted via the dynamic tracer kinetic model method and directly relates to retinal vascular permeability,” the researchers described in their paper. “This value represents the preclinical biomarker, retinal vascular permeability.”
The three diagnostic groups were found to have significantly different permeability. Despite having no clinical signs of retinopathy, the mean rank of average vascular extraction fraction was significantly higher in diabetes patients with no clinical signs of retinopathy patients compared to healthy controls. Other metrics also showed differences that researchers were able to align with disease states.
“This may have significant clinical implications considering there is currently no other retinal imaging device capable of detecting the subtle differences in retinal vascular permeability in patients with diabetes and no signs of diabetic retinopathy and controls,” the researchers concluded in their paper. “Such findings may help elucidate which of this patient type is more likely to progress to NPDR in the future. This is an aim of the larger clinical study.”
| Click here for journal source. |
Vavrek SR, Nalbant EK, Konopek N, et al. Retinal vascular permeability in diabetic subjects without retinopathy compared to mild diabetic retinopathy and healthy controls. Ophthalmol Sci. October 25, 2024. |

