So, consider these ideas to raise your level of patient care—and raise optometry’s profile in the health care community.
If you have hospital privileges,
bedside consults are not difficult and can provide critical
information. Here, Randall Thomas, O.D., M.P.H., evaluates a hospital
patient.
Acquire Hospital Privileges

We learned a long time ago that the medical/clinical evaluation we perform in our offices can also be done on mission trips, in nursing homes and, yes, in hospital settings. Our hospital center has a dedicated “eye room” in its emergency department, and we generally see ambulatory patients there.
One particular patient was admitted to the ICU with fungemia, and the consult request was to rule out fungal retinitis. Fortunately, the patient’s dilated eye exam at the bedside was entirely normal. While more thorough assessments can be performed with slit lamp biomicroscopy/ophthalmoscopy, bedside consults are relatively easily done and can provide critical information about the patient to the medical team.
Hospital eye services are clearly most needed in rural areas; however, O.D.s in urban or suburban areas (such as ours) can also provide essential eye consultative services that meet an important public health need. We encourage those of you in locations where the provision of eye care in hospital settings holds merit to pursue hospital privileges. (Download the AOA’s “Optometric Hospital Privileges” at
www.aoa.org/documents/HospitalPrivileges.doc.)
The Plaquenil workup is simple: best visual acuity; a standard
white target 10-2 visual field; and dilated ophthalmoscopy.
Photo-document macular tissues that are in any way abnormal. Plaquenil
has the potential to be retinotoxic, particularly in smaller people
(typically shorter-statured persons who have a lean body weight of less
than 135 lbs.) because the risk is quantified in a “drug-to-body
weight” relationship.
Plaquenil Clinical Evaluation
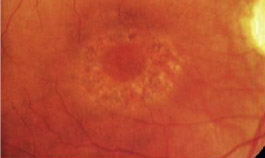
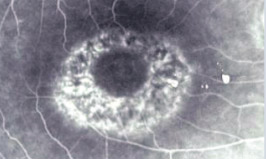
Plaquenil maculopathy.
Communicate with Other Docs
True story: A rheumatologist moved into our community. He has a brother who is an optometrist in New York, so the rheumatologist knew that his patients could see their own optometrists for Plaquenil (hydroxychloroquine, Sanofi-Synthelabo) retinotoxicity evaluations. Indeed, for a while he sent them to their optometrists for these evaluations—but he no longer does so.
Why? Very simply, the rheumatologist said that O.D.s did not send him reports on his patients’ eye/vision status. So, he now sends his Plaquenil patients to ophthalmologists, who dutifully and consistently send him timely reports.
Why do doctors of optometry often fail to communicate with other physicians? Perhaps some rheumatologists refer their Plaquenil patients to ophthalmologists for evaluations because they’re not aware of the scope and depth of services that O.D.s are trained to provide. If this is the case, we need to proactively educate those doctors and our patients about our complete competence to assess patients for hydroxychloroquine retinotoxic expression.
And, if rheumatologists are unaware of the level of care optometrists customarily provide, then certainly other specialists and primary care physicians are equally misinformed about what we do. For example, endocrinologists may not realize we can evaluate their patients for diabetic retinopathy.
In our practices, we use two forms: one for our Plaquenil evaluations and one for our diabetic eye evaluations. (Both of these forms can be downloaded and modified to suit your individual needs via our website, www.eyeupdate.com.) Other than these two forms, we dictate letters to our referring physicians.
The time has come for the profession of optometry to more fully and comprehensively communicate with the rest of the medical community. We need to let our patients and fellow physicians know that we are alive, well, and fully competent to evaluate our shared patients for a wide variety of clinical conditions.
 Abandon the Air Puff
Abandon the Air Puff
Let’s face it, most patients dread the air-puff tonometer. (The cartoon at left from our colleague, Scott Lee, O.D., in his entertaining book, Sight Gags: Cartoons for Eye Doctors and Their Patients, tells the tale.) Although the air-puff has served as a reasonable IOP “screening device” for many years, it is not at all patient-friendly.
We have waited nearly 30 years to see a technology evolve that makes the air-puff tonometer obsolete. In a busy contact lens-oriented practice, the use of drops, especially those containing sodium fluorescein, is not conducive to patient flow.
Finally, the Icare Rebound Tonometer (Icare Finland) has met all the elements to update and replace the air-puff tonometer. It is a very lightweight, portable, handheld device. Patients are grateful to no longer have to endure the air puff. Also, in most patients, its IOP readings correlate well with those of Goldmann applanation tonometry, the gold standard.1 This is another excellent way to upgrade your practice and enhance the quality of patient care. (Incidentally, we were fans of this device long before we became consultants for the company, not the other way around.)
In-Office ‘Retinal Specialist’
Pick up any ophthalmology journal from the past five years, and you’ll find at least one article about the diagnostic prowess of ocular coherence tomography (OCT). There is no debate that this technology is, to date, the most spectacular invention for assessing tissues of the posterior pole. OCT can quantify the thickness of the retinal nerve fiber layer and the thickness of the macular tissues. Some authors have said the OCT is similar to having a medical retinal subspecialist in your office. Furthermore, the utility of IV fluorescein angiography has dramatically decreased since the advent of OCT.
There is a lot of marketing energy being expended on time domain vs. spectral domain technology. Clearly, spectral domain image acquisition is superior to that of time domain images. But, for all clinically practical applications, both devices are very sufficient.
Our key advice is to plan to acquire one of these high-technology instruments as soon as you can afford it. OCT does represent the highest diagnostic technology currently available. Every O.D.’s office could offer enhanced patient care with this wonderful instrument. We urge you to carefully research these awesome technologies.
Pick Up a Pachymeter
In 2007, a panel of the World Glaucoma Association considered ways to measure IOP accurately. In particular, the panel identified the measurement of central corneal thickness as crucial. This international body of experts declared that corneal pachymetry is essential in the quantification of “risk assessment” for “glaucoma suspect” patients. Despite this, nearly 30% of optometrists do not have an instrument to measure corneal thickness, according to Review of Optometry’s recent technology survey.2
While we place great value on our GDx and OCT instruments, we find the central corneal thickness measurement provided by corneal pachymetry is even more important (and much less expensive) than these other beloved technologies. The truth is, having both corneal pachymetry and nerve fiber layer analysis is highly desirable, but we hold that pachymetry is absolutely essential. It does not make any clinically significant difference which pachymeter you acquire—they all perform well.
So, if you don’t have one, we urge you to get a corneal pachymeter. Without it, thorough risk assessment for glaucoma cannot be accomplished accurately or adequately.
Computer Lenses—Cheap
How many times do we see patients with complaints that their eyes and neck hurt while performing computer tasks? Computer vision syndrome is almost an epidemic.
A very simple answer for many of these patients is a sort of “drop-in” trifocal lens design known by the brand name PC Peekers. This supplemental lens device just drops into place behind a patient’s standard pair of glasses. PC Peekers are very cost effective––about $30 each. The +1.00D “trifocal” power gives much-improved clarity and comfort to many patients with these computer-related complaints. Our patients love them.
Check Blood Pressure
We are privileged to help teach family physicians during their formal residency training. One of the things we diligently teach them is how to quantify cup-to-disc ratios. In this manner, family physicians can begin to play a significant role in eye care by screening the citizenry for glaucomatous optic neuropathy and directing appropriate patients to us.
For our part, we can play a significant role in “family medicine” by having our staff members routinely assess patients’ blood pressures. This would be an enormous public health benefit and, beyond the altruistic outcomes, it would portray optometrists as a more fully integrated team player within the health care delivery system. Also, it would put us “on the radar” of family physicians in our communities as we direct our patients to them. Before long, you may find that you’re commonly comanaging or even “sharing” patients. It can be done, but it will require a sustained, protracted and consistent effort.
Many types of advanced technology blood pressure assessment devices are now available. A colleague at a recent lecture showed the Omron device as her favorite. It is available as a “wrist” device or an “arm” device. Each is less than $100. Choose any device you deem best suited for your practice, and one that is both patient- and staff-friendly.
True Continuing Education
“Group lecture,” i.e., a speaker and an audience, is not truly an effective format to improve one’s knowledge and skill level.3 A much more effective method involves a learned person (you) reading professional journals on a consistent, monthly basis. If an O.D. truly aspires to “continued competence,” it is best accomplished through this monthly “feeding of journal food.” Feeding oneself via the journals is how great knowledge is acquired.
Sadly, many of us were never “trained” to read the journals consistently, and equally sad, many state boards have no provision toward credit for relicensure by reading such journals. Nevertheless, we have an obligation to ourselves and to our patients to be well informed (i.e., well read) clinicians.
Three of the most prestigious and highly read journals—Ophthalmology, American Journal of Ophthalmology and Survey of Ophthalmology—are available through one website: www.ophsource.com.
We urge you to contemplate how to enhance the scope and quality of your patient care services. If optometrists can integrate the measures and technologies we espouse in this article, we will raise the level of optometric patient care as well as optometric recognition and acceptance within the entire health care system.
Drs. Melton and Thomas lecture extensively on eye disease and ocular pharmacology. They are the authors of Review of Optometry’s Clinical Guide to Ophthalmic Drugs. They are paid consultants for Icare Finland, but otherwise have no financial interest in the products mentioned.
1. Abraham LM, Epasinghe NC, Selva D, Casson R. Comparison of the ICare rebound tonometer with the Goldmann applanation tonometer by experienced and inexperienced tonometrists. Eye. 2008 Apr;22(4):503-6.
2. Murphy J. ‘New technology pays dividends.’ Rev Optom. 2009 Aug 15;146(8):36.
3. Davis D, O’Brien MA, Freemantle N, et al. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999 Sep 1;282(9):867-74.

