 |
An 18-year-old male college student presented early on a Monday morning to his hometown eye clinician in New York City with a one-day history of what he believed was likely a corneal infection after being scratched in his left eye by the nose of his beloved puppy. He was a low myope who occasionally wore contact lenses (CLs) for driving and in class but was not wearing them at the time of the incident. However, he immediately recognized that inserting his CLs after the scratch from the nose of his dog would not be wise.
At presentation, he noted mild discomfort in his left eye that had not changed since the previous day. His unaided VA was 20/25 in each eye, which improved to 20/20 with a pinhole. Biomicroscopy revealed a 2mm abrasion slightly nasal to the visual axis in his left eye only, which did stain with fluorescein dye. Intraocular pressure measurements were not taken. His record contained a sketch of the abrasion, but anterior segment photos were not obtained. The left eye was slightly more hyperemic than the right eye. There was no anterior chamber reaction in either eye. The remainder of the external exam was normal, as was the undilated fundus exam in both eyes. The diagnosis was a mild corneal abrasion in the left eye, and the clinician decided to prescribe an antibiotic/corticosteroid drop (Blephamide, Allergan) in the left eye QID for five days.
A follow-up exam was scheduled the next day, but no improvement in symptoms or clinical exam were noted. A second follow-up exam the following day yielded the same findings. Because of the failure to improve, the patient was seen two more times, but the exam results were essentially unchanged. On Saturday morning on the sixth consecutive daily visit, the eye clinician observed what he thought might be a very small and shallow infiltrate at the same location of the initial lesion. After discussing the options with the college student, the patient was sent to the emergency department (ED) of a large hospital, requesting a corneal culture. A consultant cornea specialist at the hospital evaluated the patient late Saturday afternoon, obtained a culture and speculated that the corneal abrasion from the dog’s nose may have contained a fungus and immediately began local and systemic antifungal treatment. The corneal culture later confirmed the presence of a fungus, specifically Fusarium.
 |
|
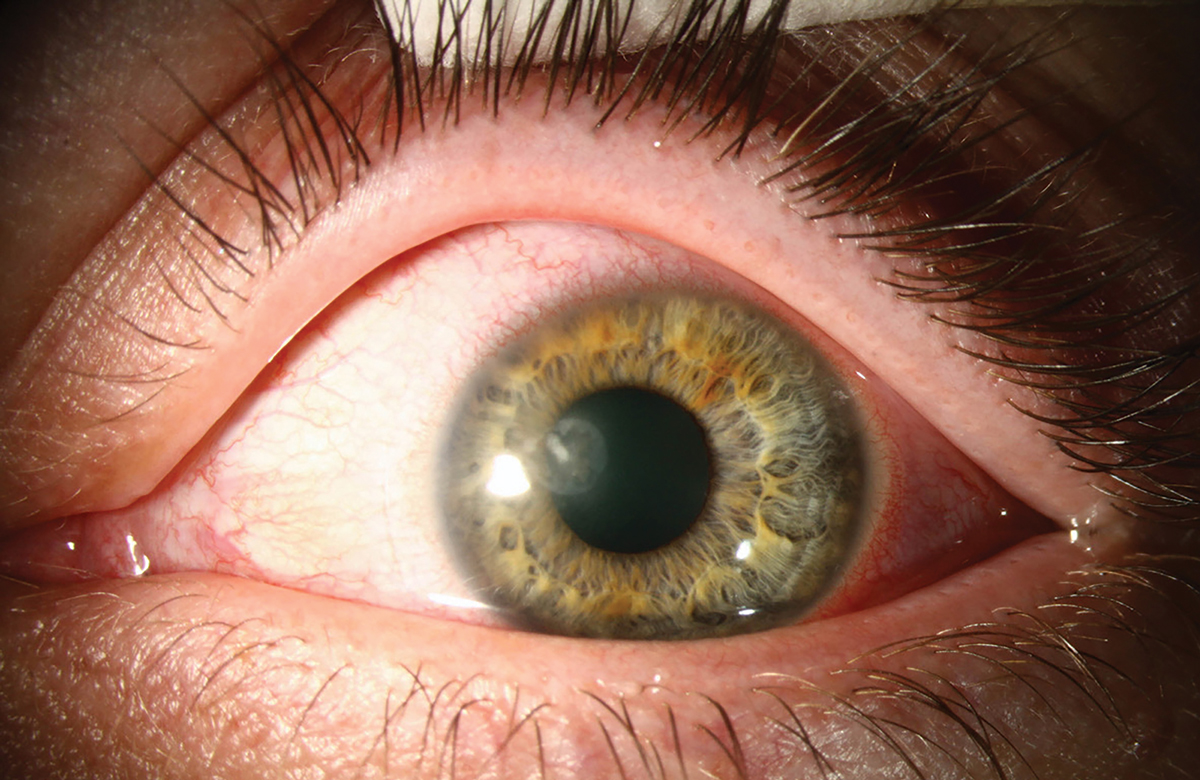
A corneal infiltrate (in a different patient) resembling an abrasion in a mildly hyperemic left eye confirmed later to be fungal keratitis. Photo: University of Iowa. Click image to enlarge. |
You Be the Judge
Considering the facts presented thus far, opine on the following questions:
- Are fungal infections from a scratch caused by a dog’s nose a common clinical encounter?
- Will treating a superficial corneal abrasion with antibiotic/corticosteroid eye drops allow the fungus (if present) to infect deeper layers of the cornea?
- Do cornea specialists recommend not to treat a corneal infection with steroids until a fungal infection has been ruled out?
- How much experience with fungal corneal infections do eye clinicians have practicing in New York?
- Regardless of the outcome, should the eye clinician not be held culpable of malpractice, since he examined the patient for six consecutive days and then referred to an ED for a corneal culture?
Follow-Up and Allegations
Although the patient was treated aggressively for the fungal infection about a week after the abrasion, the patient’s condition worsened. After three corneal transplants and two glaucoma procedures, the patient still had profound loss of vision. Additional surgery was being contemplated. The eye clinician who provided the care for six consecutive visits was sued for misdiagnosis, not considering a fungal contamination, treating the patient with antibiotic/corticosteroid eye drops without first ruling out a fungal infection and failure to refer to a cornea specialist in a timely manner. The specialist who performed the three corneal transplants was also sued for incompetent surgery.
Opinion
I (JS) was requested to review all the available information, including the surgical notes and most recent exams. Prior to completing my review of the numerous documents, reading several of the depositions that had already been obtained, review of the literature and furnishing an opinion, the case was settled for an undisclosed substantial amount against the eye clinician and the cornea surgeon.
 |
|
A corneal infiltrate with feathery edges in a red eye of a different patient proven to be due to a fungal infection. Photo: University of Iowa. Click image to enlarge. |
Comments
Fungal keratitis is typically a slow, relentless corneal infection that can easily be misdiagnosed as a bacterial infection, which accounts for the majority of the microbial corneal infections. Suspicion should be high in cases of trauma with vegetable matter and around the holiday season, as Christmas tree branch–induced abrasion has been suspected and confirmed in a significant number of cases. Vegetative ocular trauma is undoubtedly the most common risk factor for fungal keratitis. In contrast, a less-than-extensive review of the world’s literature yielded virtually nothing about a corneal abrasion from a dog’s nose resulting in a fungal corneal infection. In most cases, eye trauma, corticosteroid use and/or contact lenses are predisposing factors.1
In the United States, incidence of fungal keratitis as the etiology of all cases of keratitis varies dramatically. In New York, only 2% of cultured keratitis cases are proven to be due to a fungus, but in Florida 35% are proven to be of fungal etiology. Eye clinicians practicing at Bascom Palmer Eye Institute in Miami report encountering corneal abrasions due to a fungus as rather routine. Fusarium species are the most common cause of fungal keratitis infection in the South; Candida and Aspergillus species are more common in northern states.
Antifungal topical agents include natamycin (Natacyn, Alcon) and amphotericin B (Fungisone, Apothecon) as well as at least five systemic medicines, but eye drops alone may have limited corneal penetration. Symptoms of fungal keratitis include foreign body sensation, increasing pain or discomfort, decrease in vision and hypersensitivity to light. But of course, these symptoms do not differentiate between fungal, bacterial and viral etiologies. Feathery margins of the corneal infiltrate and elevated edge are more helpful signs for the differential diagnosis. Many conservative cornea specialists advise against using a steroid eye drop until a fungal infection has been ruled out, especially if the history yields any evidence of a possible fungal infection.
In another illustrious case, a woman working at Disney World in Orlando presented with a history of “dirt” in her eye kicked up by an elephant. This patient was also treated with an antibiotic/corticosteroid drop with similar disastrous results. It appears that the topical steroid allows the fungal infection to invade the corneal stroma even though this may go undetected with a biomicroscopic exam. The steroid helps mask the symptoms while, simultaneously, the condition worsens.
In the real world, combination eye drops containing an antibiotic and a steroid are enormously popular and effective in many cases. However, if the history in any way suggests a possible fungal infection, beware.
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.
1. Moon C. Fungal keratitis. EyeWiki. eyewiki.aao.org/fungal_keratitis. November 9, 2023. Accessed March 20, 2024. |

