 |
A 20-year-old Caucasian male college freshman presented for his first eye exam complaining of blurred vision in his right eye, most noticeable after an hour or so of near work. The patient mentioned to the technician that the blurred vision was a new symptom, but this comment was not entered into the record. The technician recorded the eye health history and general health history as negative. The tech measured unaided visual acuity as 20/25- OD and 20/20 OS. Pinhole VA was not recorded. The refraction performed by the tech was +0.50D sphere OD and plano OS. Near testing revealed an add of +1.00D OU. VA did not improve, and again pinhole VA was not recorded. The tech performed a visual field screener with a Harrington-Flocks Multiple Pattern Screener, which revealed a mild defect in the right eye only.
The ophthalmic clinician later performed an external exam, a biomicroscopy and an undilated fundus exam, all of which were recorded as normal in each eye. The clinician prescribed reading glasses incorporating a +1.50D sphere OD and a +1.00D sphere OS to be worn for extended near work. The clinician arrived at the diagnosis of mild amblyopia OD and recommended a re-evaluation in two months.
About 10 days after wearing the reading glasses for all near work, the patient returned without an appointment and complained to the receptionist that the reading glasses were not helping at all. It was a busy day in the office, and the receptionist told the college student to wear the glasses for at least two weeks and then call for an appointment if there was still a problem. The patient later reported that the receptionist said, “It’s your first pair of glasses; you just have to get used to them.”
Frustrated by the blurred vision that the patient thought might be worsening in his right eye, the college student decided to see another eye doctor who was recommended by his girlfriend, who was concerned about his vision. Best-corrected VA was now measured at 20/100 in the right eye and 20/20 in the left.
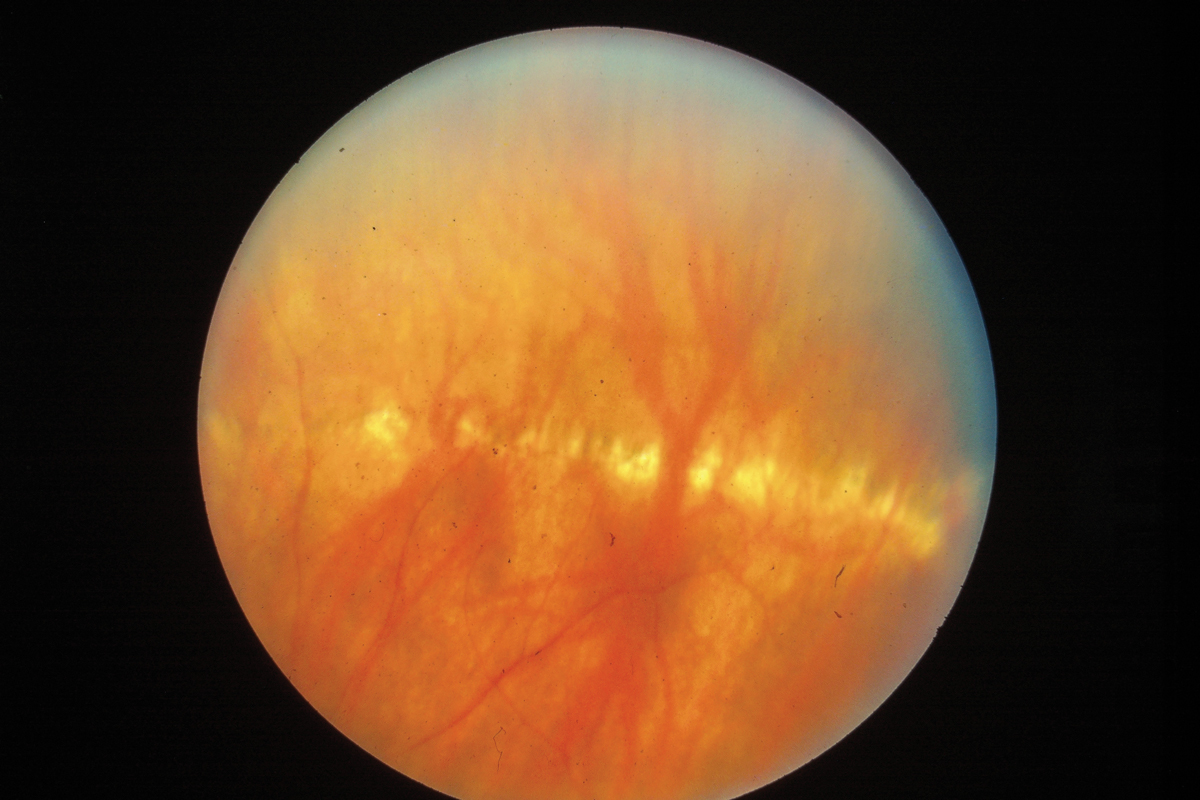
A dilated fundus exam (DFE) revealed a lesion surrounding the optic disc in the right eye, extending to the macula with possible macula hemorrhaging. The peripheral retina revealed numerous small, punched-out circular scars in both eyes. This clinician arrived at a tentative diagnosis of presumed ocular histoplasmosis syndrome (POHS) and arranged for a retina consult two days later.
 |
|
Linear array of histo spots in the peripheral retina in a different patient. Click image to enlarge. |
You Be the Judge
Considering the facts presented thus far, opine the following questions:
- Was the diagnosis of amblyopia supported on the first visit?
- Without a constant unilateral strabismus and/or significant anisometropia, was amblyopia a plausible diagnosis?
- Was the receptionist justified in her recommendations to the patient?
- Do the doctors in the practice have responsibility for their ancillary personnel in a case such as this?
- Should ancillary personnel be making “professional” decisions?
- Did the doctor really conclude amblyopia was the diagnosis, or was this just for billing purposes?
- Could a dilated exam on the first visit or ultra-widefield imaging have alerted the clinician to the probable diagnosis at an early stage prior to vision loss?
Outcome
The retina specialist confirmed the triad of findings typical of POHS: peripapillary abnormalities, choroidal neovascularization (CNV) in the macula and punched-out circular lesions in the periphery. These histo spots are quite helpful in arriving at a diagnosis and support the need for a DFE and/or ultra-widefield images. This inflammatory condition occurs when the Histoplasmin capsulatum fungus invades the eye.1 Unlike toxoplasosis, vitritis and iritis virtually never occur in histo.
CNV was confirmed with fundus fluorescein angiography, and the patient was treated with an argon laser. One of us (JS) reviewed the case and evaluated the patient after the completion of the argon laser intervention. Best-correctable VA dropped to below 20/400 OS, and ophthalmoscopy and fundus photography revealed a one disc diameter pigment lesion, visible sclera, and an irregular ring around the disc. Disc drusen may have been present in the right eye but the VA reduction is due to the macula lesion secondary to the CNV and the laser intervention. Note that this case occurred prior to the widespread availability of spectral-domain OCT, so OCT sections through the macula were unavailable.
Some patients with POHS have the histo spots but never develop the maculopathy, so the triad of findings is often not complete. If you encounter a patient without symptoms but with histo spots and a ring around the disc but no maculopathy, the patient should be warned about the possible development of vision loss due to an active macular lesion. Such a patient should be followed more carefully and taught how to use an Amsler grid. Clinicians who monitor their age-related macular degeneration AMD patients with the ForeseeHome device (Notal Vision) for the early detection of the conversion of dry to wet AMD may consider this home device, which has proven to be more sensitive to early detection of CNV than the Amsler grid.
The case settled against the first clinician and the practice prior to a jury trial for a reported quarter of a million dollars.
 |
|
Scattered histo spots in the mid-periphery of another patient. Click image to enlarge. |
Liability Considerations
Vicarious liability, or imputed liability, is a legal rule that holds a person or company responsible for actions committed by others or their employees. Such liability can apply to any business enterprise, including healthcare facilities and hospitals. Rarely does a receptionist or technician get sued, but their supervisors do. In this case, the technician failed to record that the blurred vision was a new symptom. This grave error could be just sloppiness or improper training.
In a previous You Be the Judge article (Diagnose Amblyopia with Caution, November 2023), the monocular vision loss in a 13-year-old was rather recent but this information was never recorded. The clinician in that case (as in this case) appeared to assume that the vision loss or blurred vision was long-standing. Hence, both clinicians arrived at the erroneous diagnosis of amblyopia. In the case of the 13-year-old patient, blindness OU was the outcome due to a one-year delay of diagnosis and treatment for a chiasmal mass. The jury in that case found the eye clinician culpable and awarded the patient and family over nine million dollars. In addition, make sure your receptionists and technicians are well trained and are not making professional decisions, such as in this case, “It’s your first pair of glasses, you just have to get used to them.”
A re-evaluation of the college student the day he returned and complained “the glasses are not helping at all” would have, more likely than not, resulted in an earlier diagnosis of POHS, earlier intervention and a better outcome.
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.
1. Roth AM. Histoplasma capsulation in the presumed ocular histoplasmosis syndrome. Am J Ophthalmol. 1977;83(3):293-8. 2. Macular Photocoagulation Study Group. Argon laser photocoagulation for ocular histoplasmosis. Arch Ophthalmol. 1983;101(7):1347-57. 3. Gabel W. Vicarious liability. J Am Optom Assoc. 1987;58(7):599-601. |

