 |
Q:
I have a patient who underwent successful cataract surgery but is best-corrected 20/30. OCT showed some macular thickening. What is going on?
“Your patient has an epiretinal membrane (ERM)!” says Julie Rodman, OD, professor and chief of the Eye Care Institute of Nova Southeastern College of Optometry. ERMs are superficial, avascular, contractile sheet-like membranes composed of glial cells, retinal pigment epithelial cells, macrophages, fibrocytes, collagen cells and laminocytes.1 When in contact with the retina, these cells proliferate and form a membrane over the surface of the retina. These membranes expand and contract, resulting in anatomic changes that include distortion and thickening of the underlying sensory retina. Subsequent visual changes including metamorphopsia and blurry vision may occur.
Various ocular conditions such as anomalous posterior vitreous detachment, cataract surgery, retinal tears, retinal vascular disease and ocular inflammatory disease may result in ERM formation.2 ERMs may also be idiopathic in nature. Their prevalence varies depending on the etiology and is reported to be in the range of 7% to 11.8%, with age being the most important risk factor.3,4 ERMs are more common in the elderly population, with an incidence of approximately 2% in individuals over 50 and 20% in individuals over 75.2 Both sexes appear to be affected equally.
 |
|
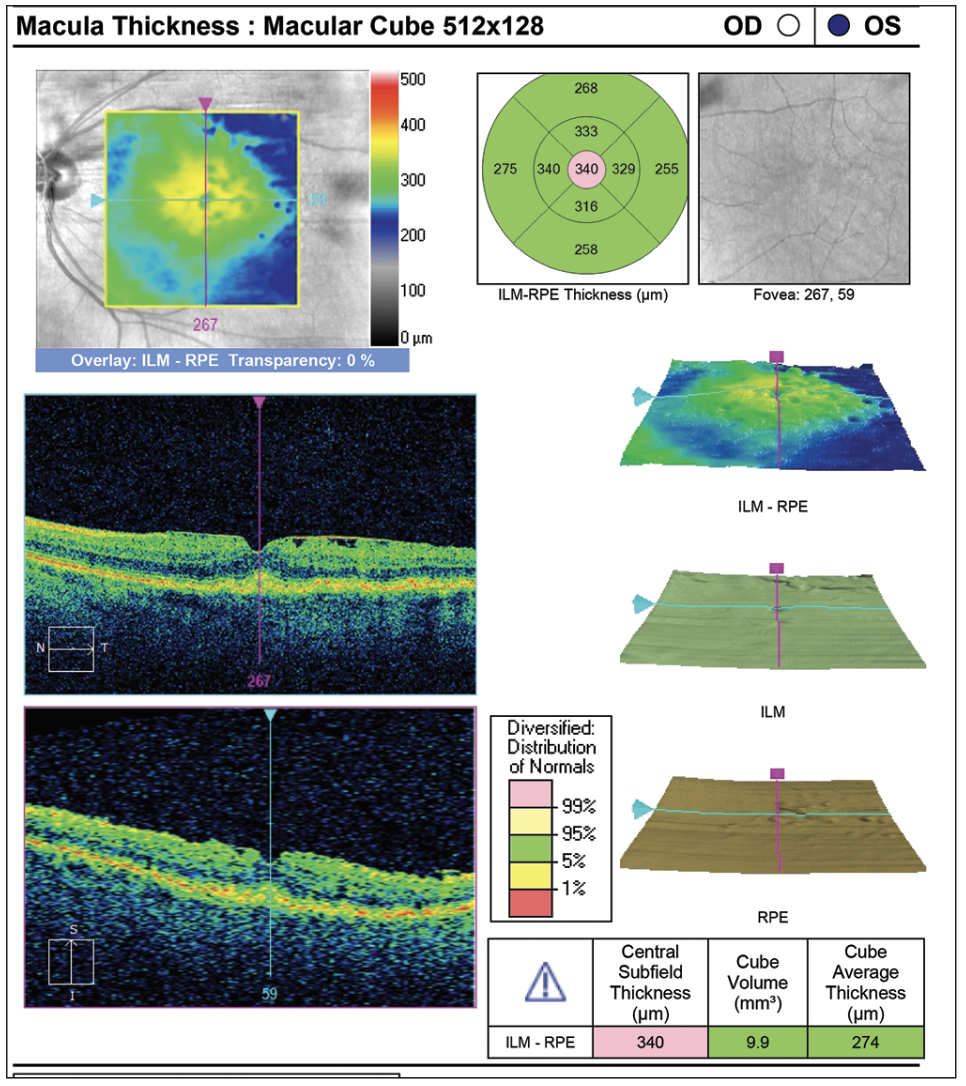
Typical ERM resulting in macular thickening and inner retinal corrugations. Click image to enlarge. |
Historically, ERM has been classified based on the degree of retinal traction and distortion. Extended periods of contraction may result in vitreomacular traction or partial- or full-thickness hole formation.4
Due to the similarity in appearance between epiretinal membranes and other entities such as exudate, combined hamartoma of the retina and retinal pigment epithelium and other proliferative vitreoretinal diseases, ancillary testing is recommended. OCT is the diagnostic testing modality of choice due to its excellent ability to identify ERM.
On OCT, ERM will appear as a hyperreflective layer superficial to the internal limiting membrane. The band may be irregular or irregular, corrugated or smooth, with or without tooth-like adherent projections Often, the foveal contour will be irregular or distorted due to the contractile forces of the ERM. Cystoid spaces and thickening may occur with significant traction. Outer retinal involvement including distortion of the photoreceptors (IS/OS junction) is correlated with visual acuity.5 Patients with ERM are more likely to develop inflammation after cataract surgery such as cystoid macular edema, neurosensory detachment and outer retinal involvement.6 Patients at risk should be treated with a topical NSAID during the entire perioperative period. Other recommended tests include the Amsler grid test and/or Watzke-Allen test. Fluorescein angiography is not routinely ordered; however, it is useful to determine if other retinal problems are causing the ERM.
To Monitor or Treat?
“The majority of ERMs will remain stable and thus can be monitored, not requiring therapy,” Dr. Rodman says. “The decision to intervene surgically depends on the severity of the symptoms including impact on daily routine.” Vitrectomy with membrane peel is the treatment of choice and is indicated in patients who have a decrease in visual acuity that interferes with lifestyle, metamorphopsia and double vision or difficulty with binocularity.7,8 Encourage patients to use Amsler grid at home routinely to monitor for changes that may occur over time and to notify their eye physician if symptoms change. Surgical removal of ERM usually results in improvement in both visual acuity and clinical appearance of the retina. Preoperative visual acuity is directly correlated to surgical outcome, where better entering acuity is linked to better overall results.9 Other factors influencing outcomes include the cause of the ERM (idiopathic have better prognosis than those correlated with other ocular etiologies), the degree of traction and length of time the ERM has been present.
“ERM is in our wheelhouse,” Dr. Rodman asserts. “Use ancillary testing as appropriate and be confident in your diagnosis.” Reassurance, education and routine monitoring are of the utmost importance. As with cataract patients, only send them to the surgeon when you determine they need or want surgery.
Dr. Ajamian is board certified by the American Board of Optometry and serves as Center Director of Omni Eye Services of Atlanta. He is vice president of the Georgia State Board of Optometry and general CE chairman of SECO International. He has no financial interests to disclose.
1. Stevenson W, Prospero Ponce CM, Agarwal DR, et al. Epiretinal membrane: optical coherence tomography-based diagnosis and classification. Clin Ophthalmol. 2016;10:527-34. 2. Kanukollu VM, Agarwal P. Epiretinal Membrane. [Updated 2023 Jul 24]. In: StatPearls. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK560703. Updated July 24, 2023. Accessed August 1, 2024. 3. Folk JC, Adelman RA, Flaxel CJ, et. al. Idiopathic epiretinal membrane and vitreomacular traction Preferred Practice Pattern guidelines. Ophthalmology. 2016;123 (1):152-81. 4. Fung AT, Galvin J, Tran T. Epiretinal membrane: a review. Clin Exp Ophthalmol 2021;49(3):289-308. 5. Govetto A, Lalane RA, Sarraf D, et al. Insights into epiretinal membranes: presence of ectopic inner foveal layers and a new optical coherence tomography staging scheme. Am J Ophthalmol. 2017;175:99-113. 6. Roh M, Kim EL, Eliott D, Yonekawa Y. Internal limiting membrane peeling during idiopathic epiretinal membrane removal: pros and cons. J Vitreoretin Dis. 2017;1(2):138-43. 7. Zafar S, Siddiqui MAR, Shahzad R, Shahzad MH. Swept-source optical coherence tomography to screen for macular pathology in eyes having routine cataract surgery. J Cataract Refract Surg. 2017;43(3):324-7. 8. Vallejo-Garcia JL, Romano M, Pagano L et al. OCT changes of idiopathic epiretinal membrane after cataract surgery. Int J Retina Vitreous. 2020;6:37. 9. Hosoda Y, Ooto S, Hangai M, et al. Foveal photoreceptor deformation as a significant predictor of postoperative visual outcome in idiopathic epiretinal membrane surgery. Invest Ophthalmol Vis Sci. 2015;56(11):6387-93. |

