 |
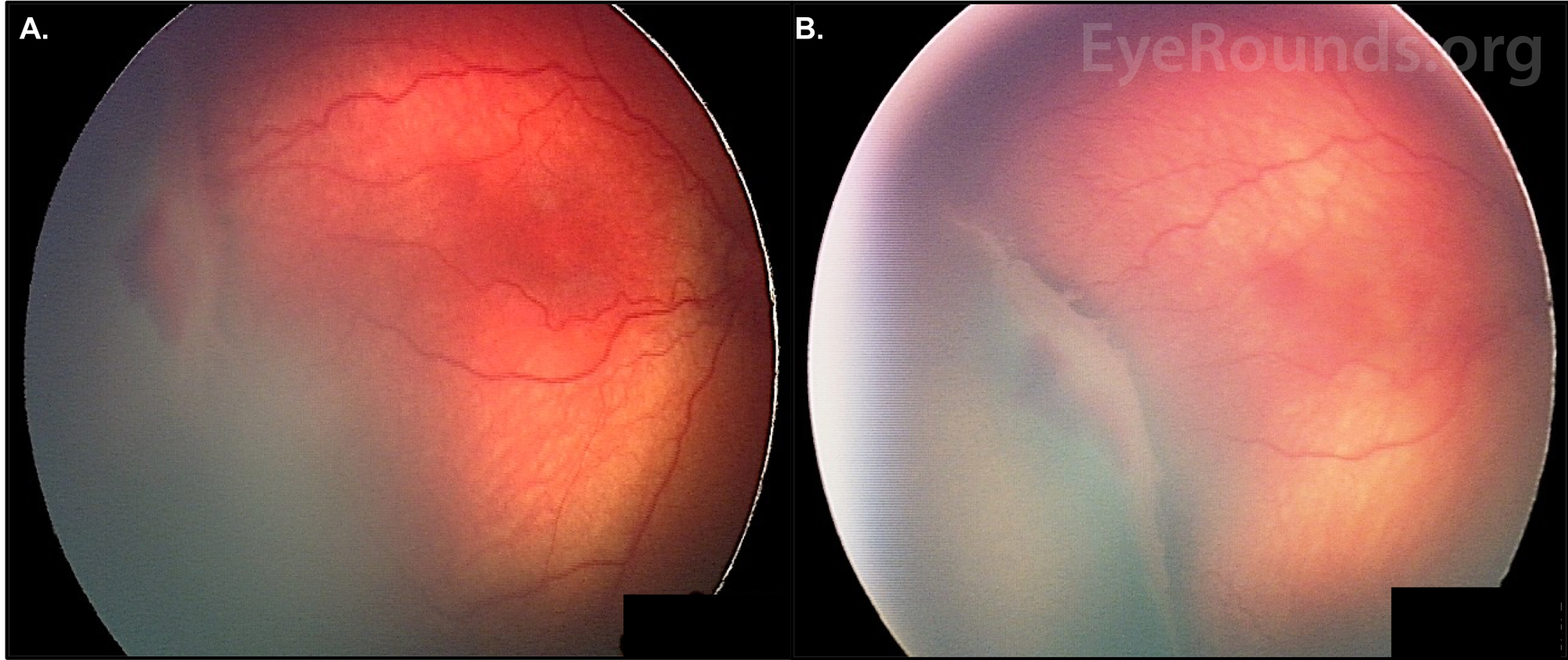
| Adding measures that would raise sensitivity of ROP testing to 100% would make sure all infants are properly screened, even if it means more infants need to be examined. Photo: University of Iowa. Click image to enlarge. |
Infants born preterm are at risk for a range of developmental issues, and the visual impairment arising from retinopathy of prematurity (ROP) can take quite a toll on quality of life, so accurate screening and swift intervention are critical. While current models to predict visual impairment catch most children, these are due for an update to include more than just weight and gestational age, says a new study in JAMA Ophthalmology. A group of investigators looked at the prognostic impact of intravenous feeding (i.e., parenteral nutrition duration or PND) on ROP, since the relationship is not well-documented. Doing so could improve prediction models to optimize disease management by helping specialists discern high- from low-risk infants.
The goal of the researchers was to update and validate prescreen and screen prediction models to include all ROP-screened infants despite gestational age, as well as to incorporate the influence of PND.
Premature infants from the Swedish National Registry born from 2007 to 2020—11,139 in all—were retrospectively assessed for ROP diagnosis. PND was studied in relation with ROP overall and cases needing treatment.
Of this large cohort, 45.5% were female and mean gestational age was 28.5 weeks. ROP developed in 29% of infants and treatment was given to 5%. Parenteral nutrition of less than 14 days was administered in 65%, while 21% had PND that persisted for longer than that time. A meaningful 14% had unknown PND status. The supplemental nutrition was additionally found to be correlated with severity of ROP, and infants that displayed 14 or more days of intervention had 84% higher odds of developing any ROP and 120% higher odds of ROP treatment than those with less than 14 days persistence. This subgroup also displayed higher odds of any ROP and of severe ROP that needs treatment.
Based on these differences, the authors conclude in their article that “continuous research on neonatal nutrition for premature babies is warranted,” since infants needing treatment was significantly higher for those needing IV nutrition greater than 14 days.1
Previous literature has showed that PND, gestational age, birth weight and length of oxygen are all independent predictors of any ROP. One study indicated PND of more than 10 days was predictive of needing ROP treatment, while another developed a prognostic model that mapped more than 13 days of PND to be a significant predictor for type 1 ROP development. It may not just be related to duration of IV feeding, but also to volume. One prior investigation found the volume of PND during week two, but not week one, related to severe ROP outcome.
The authors found in this study that PND was also greater in girls than boys, especially with lower gestational age, when ROP needs treatment more often. The disease progressed faster for those who needed IV treatment longer, independent of gestational age. Because of this, they argue that “further investigation of the mechanism behind early sex-specific effects of parenteral nutrition and its relation to intestinal and neovascular development as well as accelerated progression of severe ROP is needed.”
In an invited commentary also published in JAMA Ophthalmology, one author points to this work’s withstanding effects. Two decades ago, their model led to using slow postnatal weight gain to surrogate for low-serum growth factors, which limits retinal vascular endothelial growth factors activity and leads to ROP, as well as initiating development of many ROP models.
This author argues, though, that this original research adds to the field where other studies have fallen short. While many previous studies have attempted to reveal other factors contributing to ROP, independently associated factors of sepsis, thrombocytopenia and nutrition only add minimal additional predictive value over models using birth weight and gestational age.
Typically these two factors alone are insufficient, since a small number of infants with greater birth weight and gestational age do develop type 1 ROP, making screening levels higher and lowering specificity.
The author posits that improving sensitivity to 100%, as this new model has, highlights that conventional criteria are not all there is to use. This model, however, can include outlier infants with type 1 ROP without subjective criterion, effectively including all who are at-risk, which could not have been achieved before using the standard two factors.
The commentary author ends with a concrete call-to-action: “We should, at a minimum, add a straightforward postnatal weight gain criterion, such as less than 200g weight gain during any 10-day period over ages 10 to 40 days, to raise the sensitivity of the ROP screening guidelines to 100%, and we can continue to use simple birth weight and gestational age thresholds, which can safely be lowered.”2
1. Pivodic A, Holmström G, Smith LEH, et al. Prognostic value of parenteral nutrition duration on risk of retinopathy of prematurity: development and validation of the revised DIGIROP clinical decision support tool. JAMA Ophthalmol. June 29, 2023. [Epub ahead of print]. 2. Binenbaum G. Retinopathy of prematurity screening—asking the proper question. JAMA Ophthalmol. June 29, 2023. [Epub ahead of print]. |

