 |
|
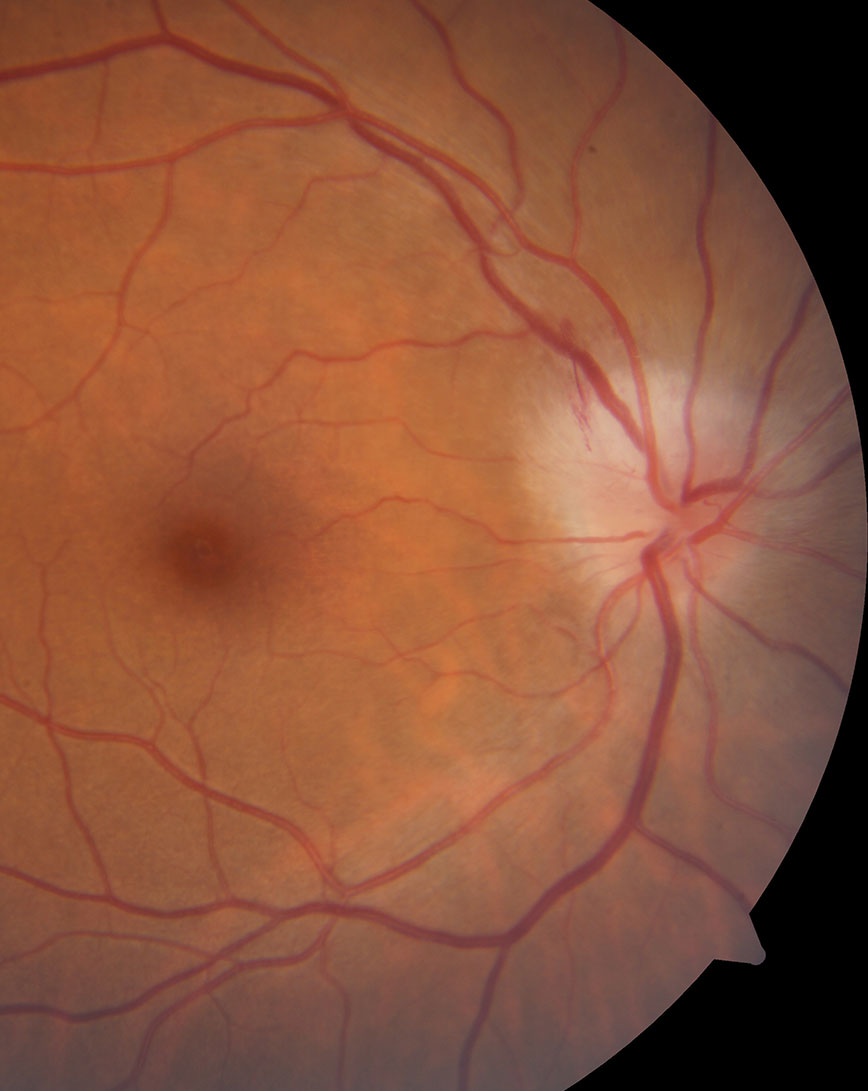
In this study cohort, optic nerve head edema always accompanied the presence of PHOMS in patients with optic neuritis. Photo: Nate Lighthizer, OD. Click image to enlarge. |
In 2020, new diagnostic criteria were developed for peripapillary hyperreflective ovoid mass-like structures (PHOMS), an OCT finding whose presence has been associated with numerous optic nerve conditions. To confirm PHOMS under these guidelines, the following must describe the hyperreflective structures: they must be strictly located around the optic disc, lie on Bruch’s membrane, induce an upward deflection of at least two adjacent retinal layers and have a signal appearance similar to the hyperreflectivity of the retinal nerve fiber layer or the ganglion cell layer.
Given that optic neuritis can induce disc changes in some patients with demyelinating disorders such as multiple sclerosis, researchers wondered whether PHOMS could be a sign of the condition using the new criteria. Their study observed that the finding wasn’t commonly seen in patients with optic neuritis; rather, they concluded that PHOMS appears to be a rare sign of optic neuritis associated with optic nerve head edema.
The team analyzed the medical files of 102 patients (115 eyes) from the OCT and Optic Neuritis study cohort. Of these, 29% of eyes had optic nerve head edema upon initial presentation, and 7% met the diagnostic criteria for PHOMS. The researchers reported in their paper, published in Eye, that all cases of PHOMS “were unilateral and occurred in eyes with optic neuritis associated with optic nerve head edema.”
The eight cases of optic neuritis with PHOMS were related to one of the following conditions: MS, Lyme disease, anti-MOG syndrome or clinically isolated syndrome, and three cases were idiopathic.
By the one-month follow-up, PHOMS had already disappeared in 75% of cases, and by three months, it had resolved in 100% of cases. The team suggested that the presence of PHOMS “over a year after the resolution of optic disc edema could suggest a non-inflammatory cause of optic neuropathy. However, this applies in cases unrelated to tilted optic discs, where PHOMS are a common finding,” they wrote in their paper.
To conclude, this analysis suggests that PHOMS, determined using updated guidelines, should not be considered a clinical sign of retrobulbar optic neuritis.
Aziria A, Philibert M, Deschamps R, et al. Are PHOMS a clinical sign of optic neuritis? Eye. January 31, 2023. [Epub ahead of print]. |

