 |
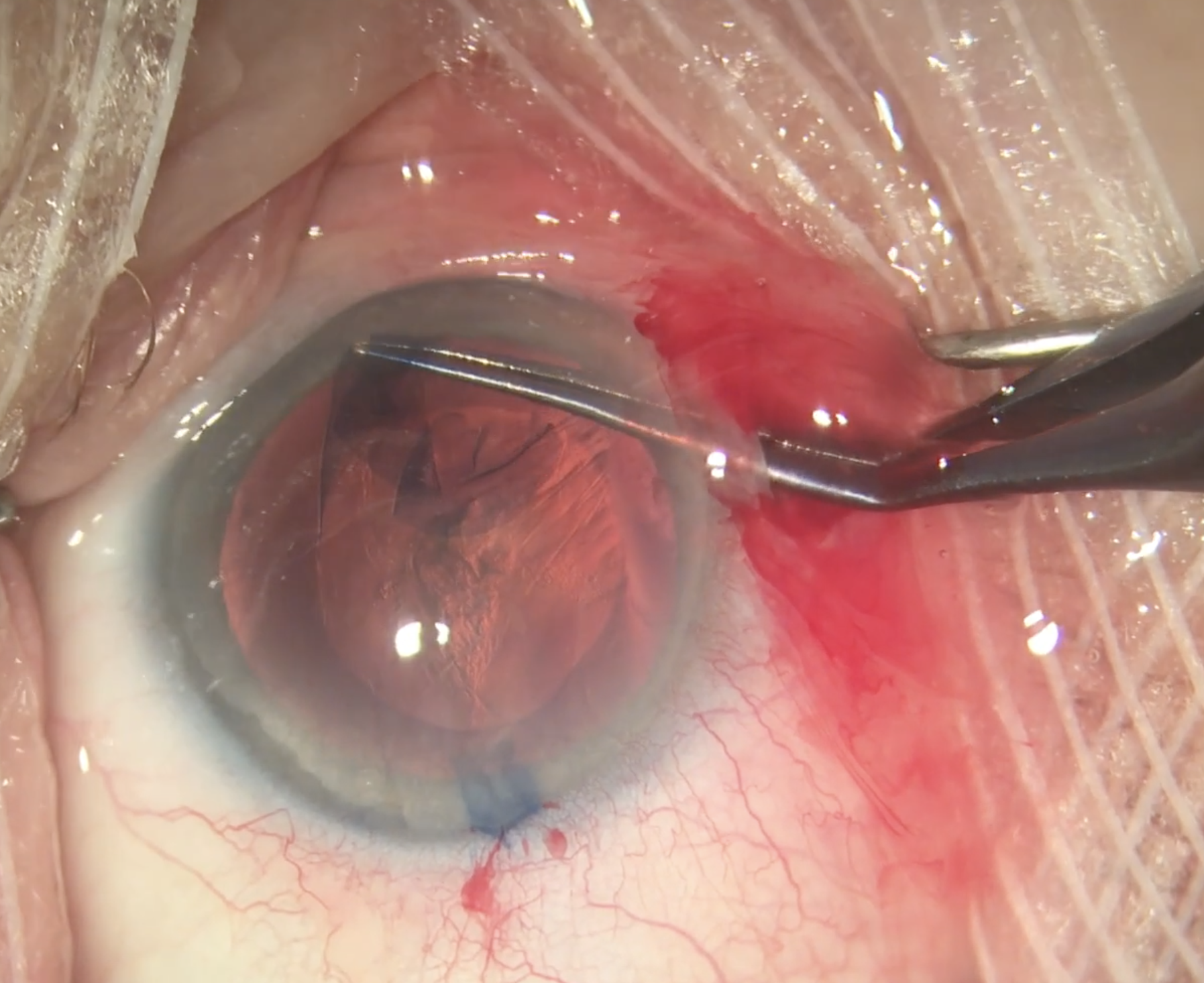
| Baseline IOP was the characteristic with the strongest relationship to IOP response failure as eyes with higher baseline IOP were more likely to maintain this reduction after surgery. Nearly all glaucoma diagnoses had greater odds of IOP response failure compared to glaucoma suspect eyes. Photo: Christina Tran, BS, and Leonid Skorin, Jr., DO, OD. Click image to enlarge. |
A better understanding of the factors associated with IOP reduction after cataract surgery and the survival of this IOP response may not only help explain its etiology but also assist surgeons when considering stand-alone phacoemulsification vs. a combined procedure. Researchers from the Bascom Palmer Eye Institute at the University of Miami explored predictors of a clinically significant IOP response, defined as a confirmed 20% or greater reduction in IOP from baseline, as well as survival of the IOP response for eyes with glaucoma and pre-glaucoma. Their multivariate analysis found baseline IOP was the greatest predictor of IOP response, with a hazard ratio of 1.48 for every 3mm Hg. Their results suggested that the causative mechanism attributed to age likely involves more than lens density because cataract diagnosis, such as total or mature cataract, was not an independent predictor of IOP response.
The researchers leveraged the size of the IRIS Registry to describe the real-world incidence and maintenance of clinically meaningful IOP reduction following stand-alone phacoemulsification for 667,987 eyes with suspected or confirmed glaucoma over a period of more than six years.
The estimated IOP responder rate was 41.3% by Kaplan-Meier analysis. Multivariate analysis demonstrated relationships between IOP response and baseline IOP (hazard ratio; HR: 1.48 per 3mm Hg), age (HR: 1.14, per 10 years), male sex (HR: 1.13), prostaglandin analog (HR: 0.88) and Rho-kinase inhibitor use (HR 1.50). The study found that 50% of IOP responders failed at a median time of 14.3 months. Multivariate analysis demonstrated relationships between failure and baseline IOP (HR: 0.75 per 3mm Hg), nitric oxide-donating prostaglandin (HR: 1.78) and Rho-kinase inhibitor use (HR: 1.73).
Eyes that were aphakic after surgery or on baseline prostaglandin medication were less likely to be IOP responders. Additionally, compared to glaucoma suspects, IOP response was more likely in cases of primary angle-closure suspect, pseudoexfoliative glaucoma and primary angle-closure glaucoma but less likely in primary open-angle glaucoma.
“Similar to predictors of IOP response, baseline IOP was the characteristic with the strongest relationship to IOP response failure, as eyes with higher baseline IOP were more likely to maintain this reduction after surgery,” the team wrote in their paper. “Nearly all glaucoma diagnoses had greater odds of IOP response failure compared to glaucoma suspect eyes.”
Given the limited long-term survival of IOP reduction from standalone phacoemulsification suggested in this study, they noted that surgeons may consider a concurrent procedure such as MIGS if there is a concern about IOP control with a patient with unfavorable odds of IOP response or survival.
“The precision and volume of large data repositories such as the IRIS Registry could be used to train predictive models that could enhance personalized medicine and aid in this decision-making process,” the study authors concluded. “These relationships may help guide surgical planning to better predict which eyes with glaucoma or pre-glaucoma may or may not have a clinically meaningful and sustained IOP reduction following cataract surgery.”
Rothman AL, Chang TC, Lum F, Vanner EA. Predictors of intraocular pressure response and survival after phacoemulsification for glaucomatous eyes in the IRIS registry (Intelligent Research in Sight). Sci Rep. 2024;14(1):19050. |

