 |
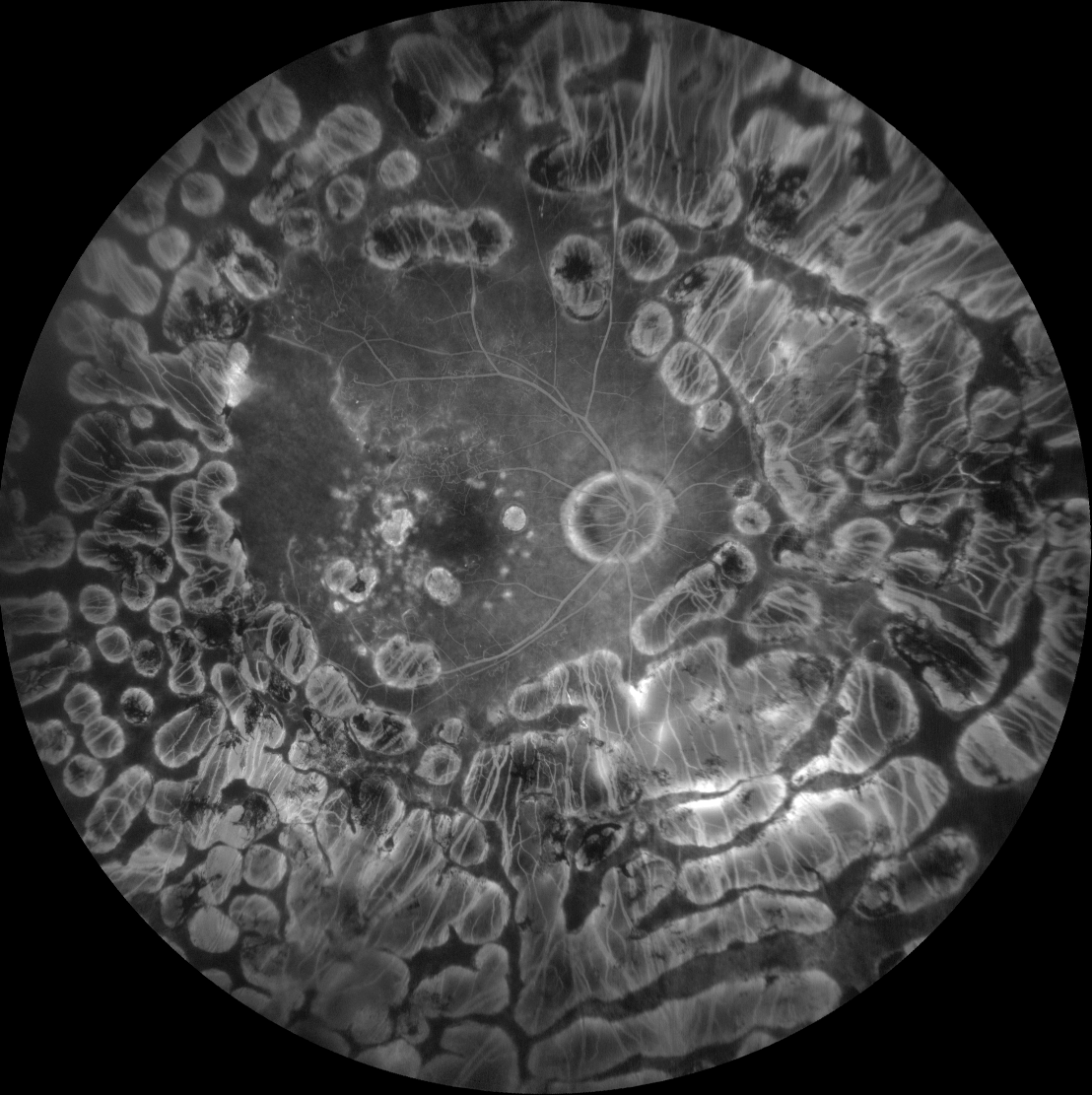
| PRP has fallen out of favor in recent years as anti-VEGF is more sparing of the retina and generally safer, with comparable results. This study showed differences in complication rates between the two. Photo: Christine Sindt, OD. Click image to enlarge. |
Data suggests that patients with proliferative diabetic retinopathy (PDR) who received panretinal photocoagulation (PRP) monotherapy were more likely to develop vitreous hemorrhage (VH) or tractional retinal detachment (TRD) and ultimately undergo pars plana vitrectomy (PPV) when compared with those who received anti-VEGF alone.
This retrospective cohort study, published recently in JAMA Ophthalmology, used an aggregated electronic health records research network to examine outcomes of PDR patients treated with PRP monotherapy vs. matched patients treated with anti-VEGF monotherapy.
Before propensity score matching, researchers identified 12,626 patients in the PRP monotherapy cohort and 10,687 in the anti-VEGF monotherapy group. Of those, a total of 6,020 patients were subsequently analyzed in each cohort.
In the PRP cohort, the mean age was 64.8 years, 50.9% were female, 28.2% were Black and 49.0% were white. Among patients in the anti-VEGF cohort, the mean age was 66.1 years, and 50.5% were male, 26.8% were Black and 50.3% were white.
Data showed that PRP monotherapy was associated with somewhat higher relative risk (RR) of PPV when compared with patients treated with anti-VEGF monotherapy at one year (RR 1.18), three years (RR 1.15) and five years (RR 1.18). Additionally, in comparison to patients who were treated with anti-VEGF monotherapy, there was a correlation between PRP monotherapy and higher rates of VH and TRD at five years, with similar associations at six months, one year and three years. Relative risks for each were as follows:
- vitreous hemorrhage: six months (RR 2.31), one year (RR 2.20), three years (RR 1.79), five years (RR 1.72)
- TRD: six months (RR 2.84), one year (RR 2.85), three years (RR 2.56), five years (RR 2.76)
“This study revealed increased risks of requiring vitrectomy in patients with PDR treated with PRP monotherapy when compared with patients with PDR treated with anti-VEGF monotherapy at follow-ups of one year, three years and five years in a large patient dataset within the clinical practice setting,” study authors noted in their paper.
“Furthermore, this study revealed increased risks of developing VH and TRD in patients with PDR treated with PRP monotherapy when compared with anti-VEGF monotherapy,” the team concluded. Additional studies are needed to explore the mechanism for differences in rates of PPV, VH and TRD between PRP and anti-VEGF therapy.”
Alsoudi AF, Wai KM, Koo E, et al. Progression to Pars Plana Vitrectomy in Patients With Proliferative Diabetic Retinopathy. JAMA Ophthalmol. June 6, 2024 [Epub ahead of print]. |

