 |
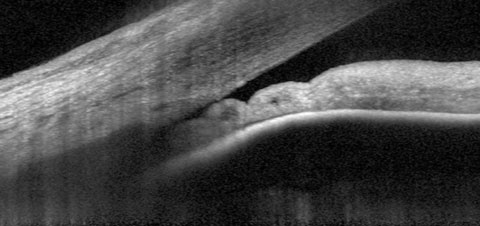
| Researchers discovered in their study that 35.2% of their narrow angle patients received only one visit with their eye care provider. Out of those patients, 52.2% were untreated for narrow angles within one year and only 14.5% were treated with LPI, drops or cataract surgery. Photo: James L. Fanelli, OD. Click image to enlarge. |
Access to health care, and especially treatment options, can vary greatly depending on a patient’s background. For patients with anatomical narrow angles, there’s a whole host of treatment options, but not every patient is treated the same. In a study recently published in American Journal of Ophthalmology, researchers observed the practice patterns and sociodemographic disparities in the clinical care of narrow angles in the United States.
The study featured patients with new diagnoses and no history of cataract surgery, prior narrow angle treatment or a prior primary angle closure glaucoma diagnosis. Among the 263,422 cases in the database used, 52,405 patients were eligible for the study.
The primary outcome was proportion of patients receiving treatment with laser peripheral iridotomy (LPI), cataract surgery or IOP-lowering drops within one year after diagnosis, explained the researchers in their paper on the study. Naturally, the cataract surgery rate would chiefly reflect visual need more so than its use as a primary intervention for narrow angle status, though that is advocated in some cases. “A secondary outcome was number of visits with eyecare providers within the one-year study period, including the index date of diagnosis.” They performed regression analysis to assess sociodemographic factors associated with treatment and eyecare visits.
Results showed that, overall, 27.7% of patients received LPI, 13.9% used glaucoma meds and 15.1% underwent cataract surgery. Researchers reported that the rate of LPI for Asian and Hispanic patients (31% and 30.2%, respectively) was higher than white and Black patients (27.3% and 25.1%, respectively). Asian, Hispanic and Black patients had a higher rate of using drops (>15.4%) compared to white patients (12.5%). However, white and Black patients had higher rates of cataract surgery (>15.3%) compared to Asian and Hispanic patients (<13.7%).
The researchers offer a litany of possible reasons for these distinctions, including cost-related barriers to healthcare access, patient mistrust of medical institutions and potential biases among healthcare providers. “The higher rates of LPI and IOP-lowering drops among racial minorities may also be related to unseen differences in ocular biometrics or other clinical factors that influence disease detection and management,” they added.
Other patient variables included in the study that were associated with higher rates of LPI treatment: residing outside the Northeast, having undergone a gonioscopic exam and obtaining care through a Medicare preferred provider organization. Those three factors also were associated with an increased rate of cataract surgery. Patients under the age of 40 had lower odds of receiving LPI while those between 50 and 79 had higher odds.
Higher rates of IOP-lowering drop use were found to be associated with male sex, older age, non-white ethnicity, history of gonioscopy and residence outside the Northeast and Midwest. Cataract surgery rates were influenced by older age, with patients over the age of 80 having the highest odds for treatment.
A low rate of gonioscopy use in the dataset was sobering. “Although the AAO recommends all patients suspected of narrow angles receive gonioscopy, only 62.1% of our study cohort had record” of undergoing the procedure prior to diagnosis, the researchers stated. However, they noted this may be an undercounting due to coding errors or use of gonio prior to the study period.
“These findings are largely consistent with prior disparities identified among [narrow angle] and primary angle closure glaucoma patients and may be related to anatomical or disease factors that are unobservable given limitations of claims-based data,” mentioned the researchers in the study. “However, the lack of understanding about causative factors highlights the need for longitudinal and multi-racial data on anatomical mechanisms of angle closure and risk factors for progression.”
Yoo K, Apolo G, Lung K, et al. Practice patterns and sociodemographic disparities in the clinical care of anatomical narrow angles in the United States. American Journal of Ophthalmology 2024. [Epub ahead of print] |

