 |
|
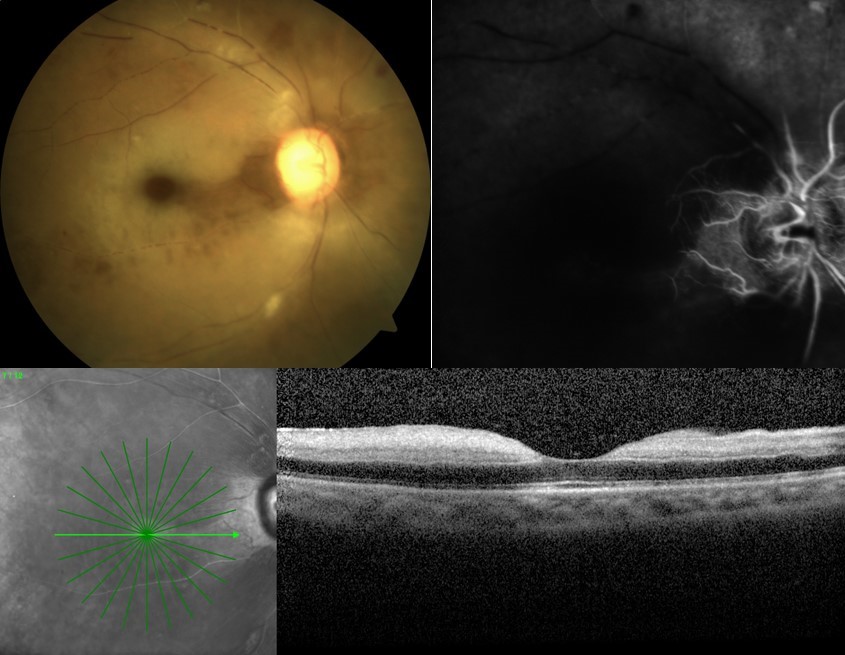
In patients with a history of cerebro-cardiovascular disease, the risk of RAO increased during the late risk period, with an incidence rate ratio of 1.19. Photo: Mo Rafieetary, OD. Click image to enlarge. |
The COVID-19 pandemic had sparked considerable interest in understanding the systemic effects of both the disease’s infection and its vaccines, leading to numerous epidemiological studies. A recent study published in Ophthalmology Science conducted a comprehensive evaluation of the association between COVID-19 infection and a range of adverse ophthalmic events by undertaking the largest self-controlled case series analysis—a work comprising the entire Korean population. The researchers found that the incidence of ocular adverse events did not increase after COVID-19 infection, except for individuals with pre-existing cardio-cerebrovascular disease, who exhibited an increased risk of retinal artery occlusion (RAO) following infection.
“Unlike traditional cohort designs that compare different groups, this study’s approach treats individuals as their own controls, emphasizing ‘when’ the event occurs rather than ‘who’ is affected,” the researchers wrote in their paper. “This methodology is inherently adjusted for all measured and unmeasured time-invariant confounders.”
The researchers divided the observation period of the study subjects into distinct risk and control periods. The risk period extended up to 24 weeks (168 days) post-infection, divided into an early risk period (eight weeks or 56 days) and a late risk period (up to 24 weeks). In cases of reinfection within 24 weeks, the risk period restarted from the new infection date, with observation censored if it concluded before the full 24 weeks. All other times during the study were considered control periods.
The study included the following rates of ocular events, early risk and late risk:
| Cases | Early Risk Ratio (0-8 wks) | Late Risk Ratio (9-24 wks) |
incident RAO | 9,336 | 0.94 | 1.02 |
retinal vein occlusion (RVO) | 103,362 | 1.01 | 1.01 |
anterior noninfectious uveitis | 201,010 | 1.00 | 1.01 |
non-anterior noninfectious uveitis | 25,428 | 0.96 | 1.02 |
noninfectious scleritis | 23,744 | 1.00 | 1.02 |
optic neuritis (ON) | 3,026 | 0.97 | 0.99 |
ischemic optic neuropathy (ION) | 69,933 | 0.97 | 1.02 |
ocular motor cranial nerve palsy | 16,335 | 1.02 | 0.97 |
Stratified analyses showed that in patients with a history of cerebro-cardiovascular disease, the risk of RAO increased during the late risk period, with an incidence rate ratio of 1.19.
The researchers did note that the diagnoses of ophthalmic diseases were based on diagnostic codes entered by physicians into claims data, preventing them from performing imaging or survey-based verification of these conditions or capturing all relevant clinical details. Nevertheless, they concluded that “this study may contribute valuable evidence to the expanding body of research on the ophthalmic complications of COVID-19.”
| Click here for journal source. |
Hwang S, Kang SW, Choi J, et al. Ocular adverse events following COVID-19 infection: a self-controlled case series study from the entire Korean population. Ophthalmol Sci. October 25, 2024. [Epub ahead of print]. |

