 |
|
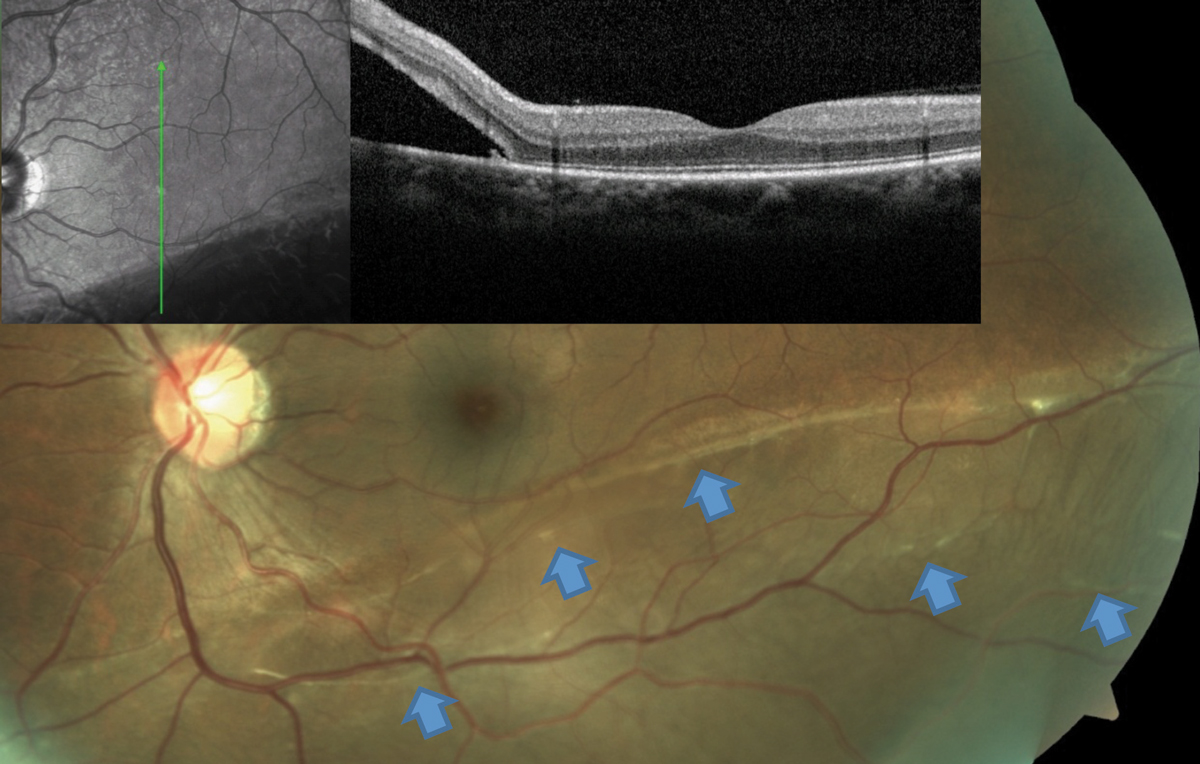
This RRD patient’s OCT image, layered over a fundus photograph, shows partial involvement of the macula, even though the patient is totally asymptomatic from this slowly progressive inferior RD. Blue arrows point to a number of subretinal bands and partial demarcation lines, a testament to the chronicity of the condition. Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
Posterior vitreous detachment (PVD), characterized by liquefaction of the vitreous gel and posterior hyaloid detachment, may herald retinal complications. Researchers reported that imaging the fellow eye—particularly the posterior hyaloid—at the time of a rhegmatogenous retinal detachment (RRD) presentation offers a “significant amount of information” about the fellow eye’s risk for RRD. Their findings were recently published in Ophthalmology.
The retrospective chart review included 1,049 patients with RRD. The researchers analyzed posterior hyaloid status on OCT and recorded baseline characteristics such as RRD family history, prior laser procedures, lens status, refractive error and lattice degeneration.
In total, 14.6% of patients had bilateral sequential RRDs during the approximately six-year follow-up period. Of the 582 fellow-eye OCT images available, 39.3% had PVD, and 51.7% had an attached hyaloid.
Among fellow eyes with PVD at presentation, 3.1% had an RRD. Among fellow eyes with an attached hyaloid at presentation, 8.2% developed an RRD during follow-up. The researchers noted that when they evaluated patients who developed a PVD during follow-up, 24.6% of those eyes had an RRD as well. Additionally, when PVD developed in the fellow eye, the researchers noted another 17.8% of eyes had a retinal tear (treated with progression to RRD).
Overall, “patients noted to have a completely detached posterior hyaloid are at a significantly lower risk of RRD than those with a visible posterior hyaloid,” the researchers wrote in their paper. Patients with visible posterior hyaloid should be monitored closely for development of PVD and counseled about the risks, they added.
They concluded in their paper that “the use of OCT imaging as an adjunct to clinical examination of the fellow eye at the time of presentation with an RRD is a useful tool to assist in risk stratification for the possibility of an eventual sequential bilateral RRD” and suggested OCT be used when counseling patients.
Wallsh JO, Langevin St, Kumar A, et al. Fellow eye retinal detachment risk as stratified by hyaloid status on optical coherence tomography. Ophthalmology. 2023. [Epub ahead of print]. |

