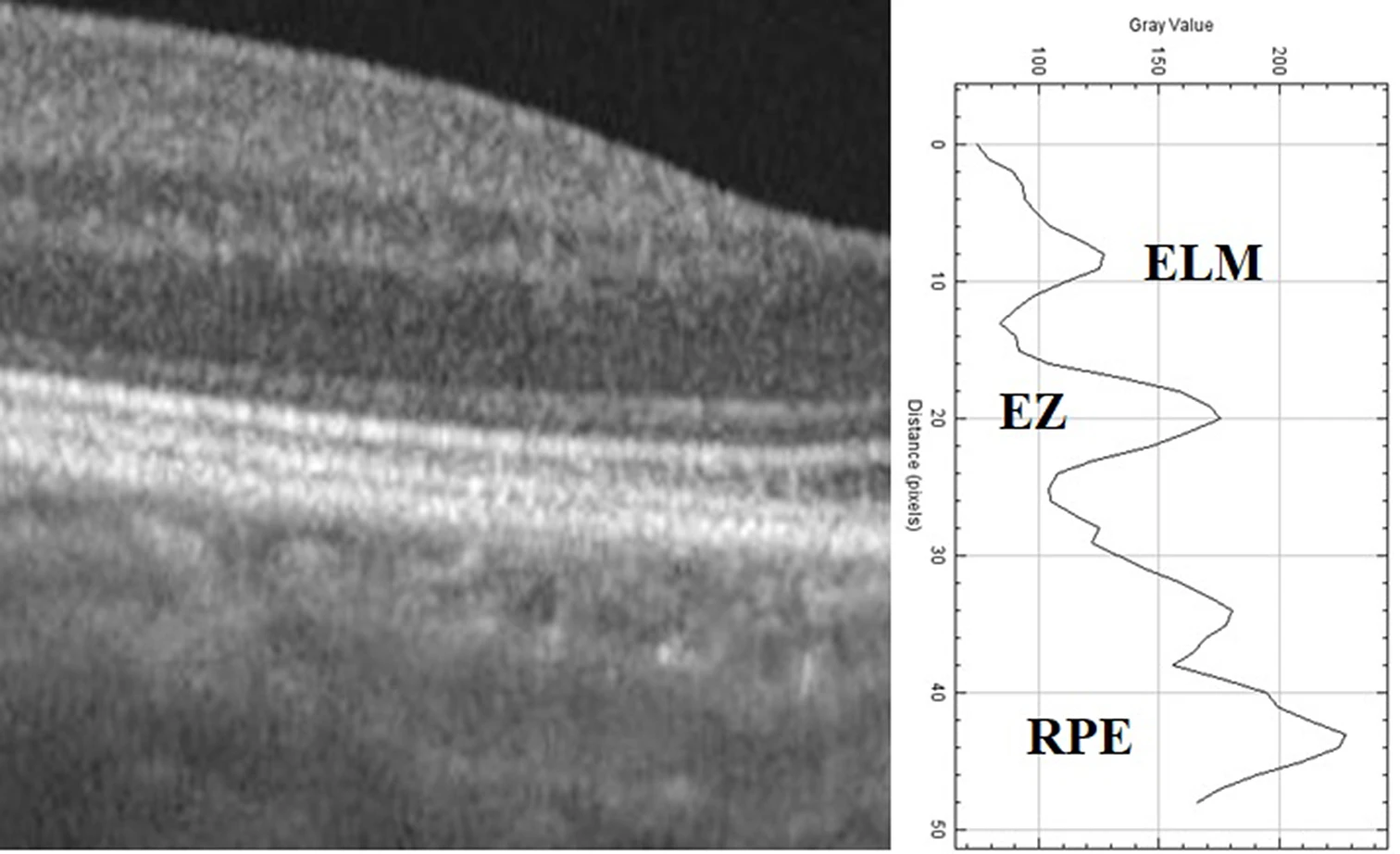
A recent study demonstrated a decrease in the reflectivities of the para and perifoveal retinal pigment epithelium (RPE), ellipsoid zone (EZ) and external limiting membrane (ELM) compared to the fovea among patients who underwent hydroxychloroquine (HCQ) treatment. The research also revealed that hydroxychloroquine use may cause increased reflectivities of RPE, EZ and ELM in the fovea, and warrants further investigation.
 |
|
This image from the study shows the peaks of the ellipsoid zone (EZ), external limiting membrane (ELM) and retinal pigment epithelium (RPE) on the reflectivity graph and grayscale OCT. Photo: Yucel Gencoglu A, et al. Graefes Arch Clin Exp Ophthalmol. June 5, 2024. Click image to enlarge. |
Prior evidence has shown that hydroxychloroquine use can lead to damage to outer retinal structures. In the current study, investigators aimed to evaluate reflectivity measurements of the RPE, EZ, and ELM within the central fovea, perifoveal and parafoveal regions.
A total of 61 patients underwent treatment with hydroxychloroquine. The analysis included 44 age- and sex-matched control group subjects. Researchers measured RPE, EZ and ELM and calculated choroid vascular index.
Data showed that RPE, EZ and ELM reflectivities in the central fovea were higher among patients who received HCQ when comapred with the control group. In the HCQ group, there was a decrease in RPE reflectivities in the temporal, nasal parafovea and nasal perifovea.
Additionally, the researchers found that EZ and ELM reflectivity in the nasal parafovea and nasal perifovea was lower in the HCQ patient group vs. the control group. “In the HCQ group, all absolute para and perifoveal reflectivities relative to the fovea decreased significantly more than in the control group,” they reported.
“Intensity analysis detects decreased ELM, EZ and RPE reflectivity in parafovea and perifovea in patients taking hydroxychloroquine. Considering the quantitative nature of this technology, it has the potential to yield objective findings in hydroxychloroquine screening for the early detection of disease,” the study authors concluded. “Further, longitudinal studies are necessary to provide additional validation for the efficacy of this technology.”
Yucel Gencoglu A, Ağın A, Colak D, et al. Decreased peri-parafoveal RPE, EZ and ELM intensity: A novel predictive biomarker for hydroxychloroquine retinal toxicity. Graefes Arch Clin Exp Ophthalmol. June 5, 2024 [Epub ahead of print]. |

