 |
Q: I have recently started to fit scleral lenses. One of my first cases is an extremely steep, peripherally thinned grafted cornea that now has ectasia. Regardless of what diameter lens and design I’ve tried, I can’t get the lens to clear the steep portion of the corneal ectasia. There’s about 0.5mm touch below the center of the cornea. Are there any frank contraindications to allowing a patient who finds the lens comfortable to wear this lens?
A: Generally, every attempt should be made to clear the apical region; however, depending on the patient, some corneal touch may be okay.
“The standard definition for a well-fit scleral lens is that it completely vaults over the corneal surface,” says Greg DeNaeyer, OD, clinical director for Arena Eye Surgeons in Columbus, Ohio. “However, a complete vault is not always achieved for patients with severe corneal irregularity or for a scleral lens that significantly decenters.”
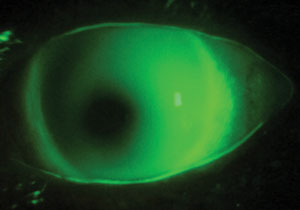 | |
| A flat-fitting scleral contact lens on a keratoconus patient. Photo: Greg DeNaeyer, OD. |
Dr. DeNaeyer points out there are studies that suggest flat-fitting contact lenses are associated with corneal incident scarring.1 Other research suggests that oxidative stress, including mechanical trauma, contributes to keratoconus.2 In the case of this particular patient, however, “the lens is probably acceptable as long as the patient is comfortable and the epithelium is healthy,” he says.“ Monitor the patient at least every six months and advise them to return immediately if they experience discomfort.”
If the patient does in fact demonstrate epithelial disruption, Dr. DeNaeyer suggests piggybacking a scleral lens on a silicone hydrogel daily disposable. “The soft lens will act as a cushion to help protect the epithelium,” he says. “Silicone hydrogel lenses maximize transmissibility, and daily disposables help to reduce care complexity and deposit-related complications.”
Christine W. Sindt, OD, clinical associate professor at the University of Iowa, notes that this issue, referred to as a tilted graft or recurrence of keratoconus, is common. Typically seen in older grafts, it occurs when the host tissue thins and stretches, she adds.
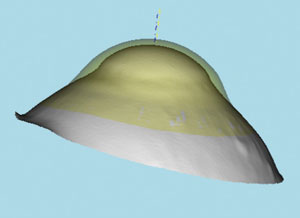 | |
| A theoretical lens on the eye with the secondary curve zone steeper than the base curve. Photo: Christine W. Sindt, OD. |
In some cases, “these grafts need to be fit with a reverse geometry design, meaning the secondary curve is steeper than the base curve,” Dr. Sindt says. “You may need to steepen and lengthen the secondary curve more or increase the optic zone size if the lens still touches the graft.”
Regardless, before even fitting the lens, Dr. Sindt recommends getting an endothelial cell count to make sure the cornea can support scleral lens wear. “It is common to experience corneal edema with endothelial cell counts under 800 cells/mm2,” she says. If the cornea is deemed healthy enough, Dr. Sindt suggests fitting a full scleral lens, rather than a mini scleral lens, since full sclerals have larger landing zones, making it easier to manipulate the intermediate curves.
1. Barr JT, Wilson BS, Gordon MO, et al. Estimation of the incidence and factors predictive of corneal scarring in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) study. Cornea. 2006 Jan;25(1):16-25.2. Kenney MC, Brown DJ. The cascade hypothesis of keratoconus. Cont Lens Anterior Eye. 2003 Sep:26(3):139-46.

