Video courtesy of Albert Cheung, MD.
 |  |
In our June column, we discussed post-op management of penetrating keratoplasty (PK)—the first corneal transplant procedure, dating back to 1905. While many cornea surgeons still perform this procedure today, it’s no longer the most common for corneal transplants. In this month’s column—part two in our mini series on keratoplasty procedures—we’ll discuss two surgical techniques that have recently surpassed PK in popularity among physicians.
The corneal endothelium is a fragile but vital layer of cells responsible for maintaining corneal clarity by transporting water out of the stroma. These cells do not replicate, leaving the cornea susceptible to developing edema should the endothelium become diseased due to conditions such as Fuchs’ dystrophy.
Full-thickness PK involves removal of healthy anterior corneal layers to treat a solely posterior disease, often resulting in suboptimal vision and leaving patients susceptible to a host of complications.
In 1956, the first report of a posterior lamellar keratoplasty was published, which involved excising only the diseased posterior corneal layers and replacing it with healthy donor posterior tissue.1 However, the idea was not further developed until the 1990s and early 2000s when a flurry of new techniques was attempted. Eventually, it was discovered that an air bubble injected into the anterior chamber can be used to push donor tissue against the host cornea.2
 |
|
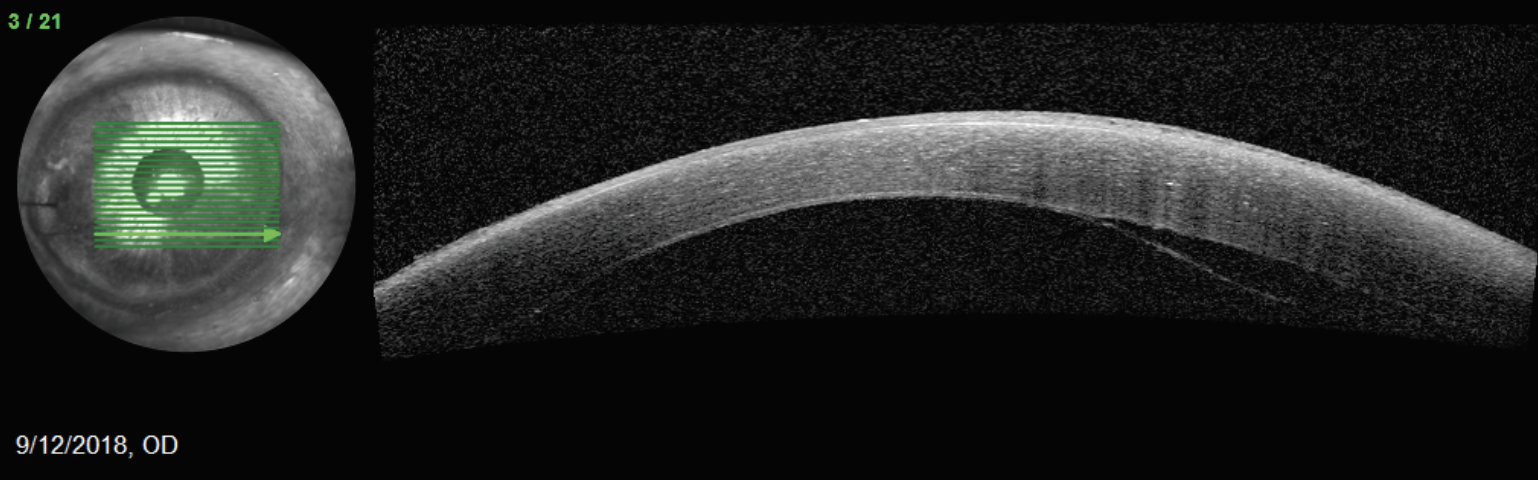
AS-OCT can be a useful tool in pre- and postoperative management. Shown here is an inferior dehiscence of DMEK graft. Photo: Walter Whitley, OD. Click image to enlarge. |
DSEK and DMEK
Various technique adjustments eventually led to Descemet stripping endothelial keratoplasty (DSEK), which has become widely accepted for treating endothelial disease given the improved visual outcomes compared to PK.3
In 2006, the first successful Descemet membrane endothelial keratoplasty (DMEK) was performed.4 This technique selectively replaces the Descemet membrane and endothelium with a donor replacement disc that is roughly 10µm thick. DMEK allows for near-complete restoration of corneal anatomy; however, the procedure does involve a different skill set than DSEK to manipulate the incredibly thin donor membrane. Due to these technical challenges, DSEK was a more popular option until recently.
Currently, DSEK and DMEK are both commonly performed in the United States thanks to the efforts of eye banks. Cornea surgeons are now able to receive donor tissue that is fully processed and may even be preloaded into injector devices. The 2023 Eye Banking Statistical report showed that DMEK was, for the first time, the most common keratoplasty procedure performed followed by DSEK and then PK.5 This highlights a recent trend toward DMEK surgery given its overall superior visual outcomes.6
Surgical Techniques
In general, endothelial keratoplasty procedures involve creating a paracentesis and main incision site. The recipient Descemet membrane and endothelium are scored 360° and a circular button of tissue is removed; this is known as a descemetorhexis. The prepared donor tissue is then inserted into the eye and apposed to recipient cornea. Temporal sutures are often used to close the main wound. An air bubble is injected underneath the graft to fill the anterior chamber. To prevent this bubble from causing pupillary block, an inferior iridectomy is performed, which may be done intraoperatively or preoperatively using a laser, or the eye may be dilated at the conclusion of the case.
Common Complications
With both procedures, graft dislocation is the most common complication.7,8 Many of these small detachments resolve spontaneously; however, more extensive cases sometimes require an additional air injection to reattach the graft. Occasionally, the grafts never clear despite graft attachment, leading to primary graft failure. Over time, the grafts undergo endothelial cell loss, and the cornea may eventually become edematous, leading to secondary graft failure.9 Graft rejection may also rarely occur.
Refractive considerations are also important. DSEK typically induces a hyperopic shift of about 1.00D to -1.50D, while DMEK induces a smaller shift of roughly 0.50D to 0.75D. Frequently, DSEK and DMEK are combined with cataract surgery, and the hyperopic shifts are accounted for during intraocular lens calculations. Very little, if any, irregular astigmatism is induced negating the need for rigid contact lenses, unlike PK.
In summary, DMEK has become the surgery of choice, as it has a greater potential to achieve excellent visual outcomes with lower risk of graft rejection. DSEK is more commonly reserved for complex cases, which pose challenges for graft unfolding.
Dr. Black graduated from Nova Southeastern College of Optometry and completed residency in ocular disease at Bascom Palmer Eye Institute. He practices at Virginia Eye Consultants in Virginia Beach. He has no financial disclosures.
1. Tillett CW. Posterior lamellar keratoplasty. Am J Ophthalmol. 1956;41(3):530-9. 2. Melles GR, Eggink FA, Lander F, et al. A surgical technique for posterior lamellar keratoplasty. Cornea. 1998;17(6):618-26. 3. Yang K, Zhao Y, Lu H, et al. Graft survival and endothelial outcomes after penetrating keratoplasty and Descemet stripping automated endothelial keratoplasty: a systematic review and meta-analysis. Exp Ther Med. 2020;20(3):2794-804. 4. Melles GRJ, Ong TS, Ververs B, van der Wees J. Descemet membrane endothelial keratoplasty (DMEK). Cornea. 2006;25(8):987-90. 5. Statistical Report. Eye Bank Association of America. 2023. restoresight.org/members/publications/statistical-report. 6. Woo JH, Ang M, Htoon HM, Tan D. Descemet membrane endothelial keratoplasty versus Descemet stripping automated endothelial keratoplasty and penetrating keratoplasty. Am J Ophthalmol. 2019;207:288-303. 7. Liang SY, Lee GA. Retained interface gentian violet ink in Descemet stripping endothelial keratoplasty. Cornea. 2012;31(1):92-3. 8. Rodriguez-Calvo-de-Mora M, Quilendrino R, Ham L, et al. Clinical outcome of 500 consecutive cases undergoing Descemet’s membrane endothelial keratoplasty. Ophthalmology. 2015;122(3):464-70. 9. Tourtas T, Laaser K, Bachmann BO, et al. Descemet membrane endothelial keratoplasty versus Descemet stripping automated endothelial keratoplasty. Am J Ophthalmol. 2012;153(6):1082-90. |

