Corneal Debridement with Diamond Burr Polishing
Doc, I’m afraid to open my eyes in the morning.” It’s a complaint that’s both shocking and severe in nature. But, it’s one that we’ve heard several times in our clinical experience.
These were extremely frustrated patients who had a long history of recurrent corneal erosions. They had already tried medical therapy, including doxycycline, Muro 128 (Bausch + Lomb), FreshKote (Focus Labs), topical steroids and even bandage contact lenses—all without success.
In these severe cases, is there another surgical option that could benefit such patients? How and when do you perfrom these more aggressive procedures?
In this article—the fourth in a six-part, print-and-video instructional series—we’ll show you how we do it.
DBD and ASP for Tough Cases
Recurrent corneal erosion (RCE) not only can be difficult to diagnose—due to its usual presentation of few clinical signs yet debilitating and recurrent symptoms—but difficult to treat, especially when it’s recalcitrant RCE.
Previous articles have discussed numerous conservative treatment modalities that are very effective in managing most cases of RCE, including hypertonic ointment, bandage soft contact lenses, oral doxycycline, topical steroids and anterior stromal puncture (ASP).1
| Simple ASP at the Slit Lamp If a patient has simple recurrent erosion from previous trauma (such as a fingernail to the cornea) and no underlying sign of epithelial basement membrane dystrophy (EBMD), anterior stromal puncture at the slit lamp can provide adequate adherence of the epithelium to the stroma. (This is assuming all other complicating factors of dry eye disease and posterior blepharitis are currently being treated and controlled as well.)
The idea behind ASP is that the punctures—no more than 250μm of penetration into the corneal surface—facilitate a slight inflammatory event that leads to minor scarring and essentially serves as a “spot weld” to better anchor the epithelium to the stroma. The procedure is best performed using an anterior stromal puncture needle rather than a bent syringe. An ASP needle comes pre-packaged and pre-bent at the tip to prevent the point from going too deep into the stroma, penetrating no more than 0.1mm. This takes the guesswork out of bending your own needle, which you could bend too much or too little. Here’s how ASP is performed: • Apply one drop topical anesthetic (proparacaine 0.5%). • Apply one drop of topical fluoroquinolone each minute for three minutes. • Test the surrounding area for poor adhesion with a Weck-Cel sponge to determine the area of treatment. Areas affected by EBMD or prior trauma—in which the epithelium is loosely adherent to the underlying basement membrane and stroma—will feel loose and will more easily separate from healthy cornea with light pressure and force from the Weck-Cel. • Using the ASP needle, apply punctures 0.25mm to 0.5mm apart to the area of loose epithelium, as well as a 0.5mm ring into the area of adherent epithelium. The punctures should be deep enough to penetrate into the anterior stroma. Scarring in the visual axis has the potential to reduce best-corrected visual acuity, so stay clear of the central visual axis when performing anterior stromal puncture. • Next, apply a bandage soft contact lens for comfort and to facilitate healing. Patients may experience mild to moderate pain in the first one to two days after the procedure, even with the bandage lens in place, due to the dozens of small punctures from the ASP procedure. Proper education usually helps alleviate the patient’s immediate concerns, and most patients feel much better one or two days later. ASP may not cure the underlying problem, so patients may still need to continue topical therapy to help control symptoms. Yet, it should significantly reduce the episodes of recurrent erosion and severe pain upon waking. | ||||||
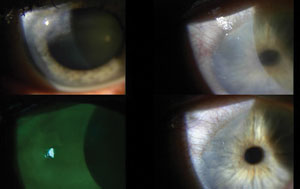 | |
| Top left: a patient with Salzmann’s nodular degeneration and epithelial basement membrane dystrophy prior to debridement. Top right: post-treatment day one with amniotic membrane ring in place. Bottom left: day one with fluorescein stain and filter. Bottom right: at one month out, the eye has almost fully healed. |
However, many of the cases seen in our surgical referral center are patients with more stubborn RCE who have failed combinations of these nonsurgical therapeutic regimens. Difficult and recalcitrant cases seem to be a result of traumatic RCE coupled with a history of EBMD. (In our clinical experience of treating recalcitrant cases that have failed conservative therapy, many seem to have concurrent EBMD that may involve the entire cornea, which likely contributes to the poorer adhesion of the epithelium in the area of previous trauma.) So, the therapeutic goal is to not only treat the current area of erosion, but also to help prevent future complications/erosions in other areas due to the underlying EBMD.
If the patient with EMBD has failed aggressive topical and oral therapy for RCE, consider surgical treatment with or without ASP. Surgical treatments include diamond burr debridement (DBD) and phototherapeutic keratectomy (PTK).
• DBD. Studies have shown that removal of the affected area of epithelium combined with polishing Bowman’s layer using a diamond burr decreases the recurrence rate (6%) when compared with debridement alone (18% recurrence).2
• PTK. This is also an excellent option to smooth the corneal surface after epithelial debridement; however, the cost to the patient is usually higher because reimbursement for use of the laser is rarely covered under insurance. Furthermore, research has shown that PTK has a slightly higher incidence of postsurgical haze and recurrence when compared with DBD.3
Accordingly, here’s a step-by-step method for DBD with ASP.
 | |
| Prepare your instrument tray ahead of time. Treat this procedure as a sterile surgery. | |
 | |
| First, apply mild pressure with a Weck-Cel sponge to remove areas of loose epithelium. Slide them off the corneal surface. | |
 | |
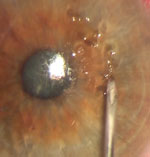
| For areas that don’t come loose as easily, use a golf club spud. Leave at least 1mm of epithelium adhered to the limbus. |
1. Discuss the Procedure
In most cases, these patients have reached the point where they’re ready for a treatment that is more aggressive because conservative therapy has failed and they’re miserable.
Discuss the risks and benefits of the procedure, and have the patient sign a consent form. (The risks include mild scarring of the cornea in the treated area, possible decreased vision if the affected area is within the visual axis, infection, pain and discomfort during healing, and recurrence—all of which are complications of not treating. Benefits include reduction or elimination of recurrence of erosions, and possibly decreasing the burden of current topical/oral treatment.)
Explain that the first couple of nights after the procedure may be more uncomfortable than the episodes of erosion, and that the patient may need oral narcotics for a couple of days.
Visual ability will be significantly reduced for a period of a week or more depending on rate of healing area and size of treatment, and whether a bandage soft contact lens or an amniotic membrane graft (e.g., Prokera, Bio-Tissue) will be used. Tell patients they can expect their vision to return to pre-surgical levels within two to three weeks.
2. Prep the Patient
Having a surgical microscope and surgical chair makes the procedure much easier because the stability of the eye is much greater and sterility is easier to maintain during the procedure. However, it can certainly be performed at the slit lamp.
Stock your surgical tray for the procedure beforehand: Weck-Cels; golf club spud; lid speculum; ASP needle; and Alger brush with diamond burr tip.
Treat this as a sterile surgery—clean the entire ocular adnexa with a swab of Betadine 5% (povidone-iodine sterile ophthalmic prep solution, Alcon), and let the patient sit for three minutes. During this time, instill a topical fluroquinolone and proparacaine—one drop of each every minute for three minutes.
Cover the non-sterile areas of the patient’s forehead, nose and cheek with a sterile drape to allow you to rest your hands during the procedure. Insert a lid speculum to keep the eyelids and lashes away from the surgical field. Also, wear gloves and a mask to maintain sterility.
3. Debride the Epithelium
To test for the areas of debridement, use a Weck-Cel sponge to dislodge and remove the areas of loose epithelium. Mild pressure will cause the affected epithelium to slide easily and freely from the corneal surface (and usually in a much larger area than the area of erosion).
Also, you may need a spud to remove small islands of adherent tissue or to dissect the edge of the affected epithelium in order to leave 1mm of epithelium adhered to the limbus. Removal of the epithelium up to or beyond the limbus can slow the re-epithelialization process.
| Two Other Indications for DBD with ASP: Preoperative Corneal Irregularity and Salzmann’s Nodular Degeneration Our referral center performs a large number of cataract surgeries and occasionally patients’ EBMD and/or Salzmann’s is significant enough that preoperative corneal measurements are too distorted to allow for proper IOL selection, especially in patients who elect toric or premium IOLs.
If you notice Salzmann’s nodules, use the spud to lift the leading edge. While grabbing and lifting the leading edge of the nodule with small-toothed forceps, use the spud to dissect the nodule from the corneal stroma back to the limbus. The nodule should “peel” off with the consistency of removing Velcro. In cases where concurrent EBMD is present, consider performing DBD with or without ASP to allow a better adhesion of the epithelium after debridement. Once the eye is healed, better preoperative keratometry and regular topography are achievable. In some cases, the procedure actually improves the patient’s vision to a point that cataract surgery isn’t necessary. |
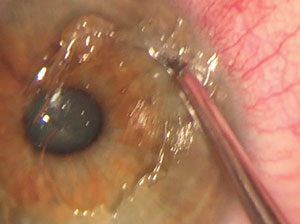
4. DBD and Polishing
Next, use an Alger brush with a diamond burr tip to gently smooth the exposed corneal surface and remove the uneven basement membrane. Be sure to hold the handle of the Alger brush so that the burr always spins toward the center of the cornea. This also allows you to smooth the edges of the remaining limbal epithelium. Only mild pressure, using smooth broad strokes, needs to be applied.
  | |
| Use the diamond burr (with rotation toward the center of the cornea) to smooth the exposed cornea. Take care to preserve the limbal cells. Roll the edge of the epithelium toward the pupil, but don’t overdo the pressure or you risk scarring in the visual axis. |
Remove any residual epithelial cells with a moistened Weck-Cel sponge. Instill a drop of topical antibiotic and a drop of NSAID on the exposed surface.
5. Add ASP
Although not conventional, performing ASP at this stage can maximize adherence of the epithelium to the stroma in severe cases of RCE, in our experience.
So, once you’ve completely removed the loose epithelium and any nodules, use the ASP needle to treat the entire exposed surface. Make a grid of punctures about 1mm apart, but stay clear of the central visual axis. Apply enough pressure to deform the corneal surface in order to penetrate the anterior stroma.
Keep in mind that because epithelium is now removed, the punctures will be slightly deeper than ASP performed with the epithelium intact. Use caution in patients who may have severe corneal thinning due to keratoconus or post-op LASIK. Preoperative pachymetry may be needed in these cases, as the ASP needle could theoretically penetrate a cornea that is 250µm or thinner.
6. Place the BSCL or AMG
At this point, place either a bandage soft contact lens or amniotic membrane graft on the surface to allow for re-epithelialization and comfort during the healing process.
We prefer to use a Prokera in our clinic if insurance allows—this provides anti-inflammatory coverage during this healing process without using a topical steroid, which can slow re-epithelialization. We’ve also noted that the Prokera seems to inhibit corneal postoperative haze formation better than use of a BSCL.
However, in instances when an amniotic membrane cannot be used due to cost or insurance coverage, a bandage contact lens is appropriate.
 |  | |
| To enhance patient comfort and promote re-epithelialization, apply a bandage contact lens soaked in fluoroquinolone. | If possible, use an amniotic membrane ring, which can be a better option than a bandage contact lens. |
7. Post-op Regimen
Prescribe a topical fluoroquinolone TID or QID to prevent infection during healing, and an NSAID QD or BID to aid patient comfort until the defect is healed. If the patient received a bandage soft contact lens, add a topical steroid TID to QID to the regimen as well. Also, Norco (hydrocodone/acetaminophen 5mg/325mg or 10mg/325mg, Watso Pharmaceuticals) will help the patient through the first couple of nights of discomfort.
Schedule the patient to return on day one to check for amniotic ring or BSCL position and healing, and then again every one to two days until complete re-epithelialization occurs. Use of sodium fluorescein stain will diffuse through the amniotic membrane graft and allow you to monitor the healing of the defect.
Once the epithelium has healed completely, remove the Prokera ring or BSCL and discontinue the antibiotics and NSAID. If the central visual axis was treated with diamond burr polishing, then continue the steroid (or add one if an amniotic membrane was used) for an additional two weeks to help reduce formation of central corneal haze. (Corneal haze is less significant when using an amniotic membrane, in our experience.)
With a small investment in time and surgical equipment, you can employ these techniques to expand the corneal treatment options for patients with RCE, EBMD and Salzmann’s degeneration. Your patient who was afraid to open her eyes in the morning will truly have an “eye opening” experience from all that you can do for them, and you’ll gain a patient for life.
Dr. Ellen is the clinical director of BVA Advanced Eye Care in Tulsa, Okla., where he specializes in the diagnosis and treatment of ocular disease.
Dr. Lighthizer is the assistant dean for clinical care services, director of continuing education, and chief of both the specialty care clinic and the electrodiagnostics clinic at the Oklahoma College of Optometry.
1. Bronner A. Peeling back the layers of RCE. Rev Optom. 2013 Jan;150(1):42-9.2. Wong VW, Chi SC, Lam DS. Diamond burr polishing for recurrent corneal erosions: results from a prospective randomized controlled trial. Cornea. 2009 Feb;28(2):152-6
3. Sridhar MS, Rapuano CJ, Cosar CB, et al. Phototherapeutic keratectomy versus diamond burr polishing of Bowman’s membrane in the treatment of recurrent corneal erosions associated with anterior basement membrane dystrophy. Ophthalmology. 2002 Apr;109(4):674-9.