 |
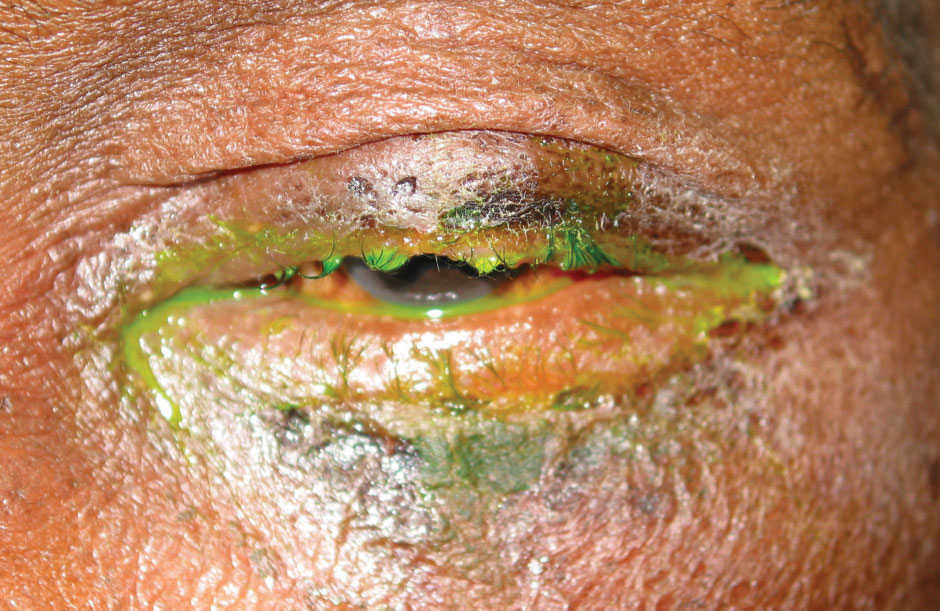
There was substantial variability in the pathogens causing acute infectious conjunctivitis in this study, with purulent discharge a common sign. This suggests that further diagnostic workup may be necessary to inform antibiotic stewardship. Photo: An Vo, OD, and Jim Williamson, OD. Click image to enlarge. |
Acute infectious conjunctivitis is a common ocular condition with public health consequences. To see if there are regional variations in the microbial etiologies of this conditions, researchers recently accessed regional variations and microbial etiologies of acute infectious conjunctivitis to guide treatment, and found that pathogens associated with acute infectious conjunctivitis varied between all sites and purulent discharge was a common sign.
A total of 52 patients with presumed acute infectious conjunctivitis were enrolled at five sites: Honolulu, Los Angeles, San Francisco, San Diego and Petah Tikva, Israel,. Patients with allergic or toxic conjunctivitis were excluded.
RNA deep sequencing revealed mixed pathogens, with virus-associated conjunctivitis predominating. Of the viral pathogens, DNA viruses were more common than RNA viruses. Also, human adenovirus-D was detected in California, while adenovirus-B was detected in Israel. Coronavirus species were seen in 50% of the cases in Hawaii. Human herpesviruses (HSV-1, VZV and Epstein-Barr) were associated with conjunctivitis in samples collected from patients at all five sites. Moreover, 32 patients presented with purulent discharge, while only four patients had confirmed bacterial pathogens.
“Consistent with prior literature on acute infectious conjunctivitis, most cases were due to viruses. The most commonly identified virus was [human adenovirus], which generally leads to a self-limited course without the need for treatment. However, this study also found variation of viral etiologies between study lines,” the authors explained in their paper for JAMA Ophthalmology.
In a previous study, human coronavirus 229E, a common strain, was detected on ocular swabs from an outpatient with acute infectious conjunctivitis. “In the current study, human coronavirus 229E was detected in Honolulu and San Francisco, suggesting it might be an underappreciated etiology of virus-associated conjunctivitis in the US,” the researchers wrote.
In Honolulu, one patient presented with primary conjunctivitis associated with SARS-CoV-2-infection and reported no systemic or respiratory symptoms. “This result is consistent with the clinical findings characterized in Madurai, India, during the COVID-19 Delta variant surge. In that cohort study, no patients with conjunctivitis associated with SARS-CoV-2 reported systemic symptoms,” the authors explained.
The prevalence of bacteria-associated conjunctivitis was low across all sites. The four documented cases were from San Francisco and Petah-Tikva. Those pathogens included Haemophilus influenzae, Fusobacterium nucleatum and Streptococcus pneumoniae. All four patients with bacterial conjunctivitis presented with purulent discharge.
“While purulent discharge is generally associated with bacterial conjunctivitis, 17 participants with virus-associated conjunctivitis also presented with purulent discharge,” the authors noted. “Thus, the specificity of purulent discharge as a clinical sign for bacteria-associated conjunctivitis is low at 39%. Given this low specificity, combined with the low prevalence of bacterial infections, clinicians local to these areas may want to limit the prescription of topical antibiotics.”
Additionally, they identified three cases of acute infectious conjunctivitis associated with HSV-1 and 2 cases associated with VZV, suggesting that some patients may benefit from antiviral treatment effective against human herpes viruses.
“Purulent discharge was a common presenting sign in this study, with a low specificity for bacteria-associated conjunctivitis, suggesting that further diagnostic workup may be necessary to inform antibiotic stewardship,” the authors concluded. “Additional research on cost-effectiveness of using RNA deep sequencing is needed to ascertain whether it is better to monitor patients clinically until resolution of disease.”
Tsui E, Sella R, Tham V, et al. Pathogen surveillance for acute infectious conjunctivitis. JAMA Ophthalmol. November 2, 2023. [Epub ahead of print.] |

