Glaucoma Pearls & PitfallsIn the July 2024 issue of Review of Optometry, our 30th annual Glaucoma Report, seasoned ODs share tips on using modern tools, technology and knowledge to provide top-notch care to your patients with this chronic condition. Check out the other articles featured in this issue:
|
As eyecare providers, we know far too well how important compliance is in glaucoma management, and it’s hard enough having patients use their drops consistently and keep their appointments.
In theory, glaucoma drops sound simple and straightforward; however, drops come with an array of troubles. Topical medications can be difficult for the patient to obtain due to several pharmacy and insurance obstacles. Many branded medications need prior authorizations and/or coupons to make them affordable. Additionally, large chain pharmacies prioritize generics over branded medications and have the ability to override our prescriptions if we do not mark “dispense as written.”
All drops also have potential ocular and/or systemic side effects that can make them intolerable or unsafe to use. Even if the drug is affordable and tolerable, sometimes the medication doesn’t reduce the intraocular pressure (IOP) effectively, leaving us trialing different agents and/or adding more drops to a patient’s regimen. Lastly, after all of the above, patients can have difficulty remembering to instill their drops or physically getting drops in their eyes.
In this day and age, no matter what stage of open-angle glaucoma (mild to severe) patients have, there are many options available that reduce our reliance on drops. These treatments—selective laser trabeculoplasty (SLT), minimally invasive glaucoma surgeries (MIGS) and sustained-release drug delivery—can potentially reduce the number of drops or eliminate the need for daily drop dosing entirely.
Historically, prostaglandin analog medications have been the first line of treatment.1 However, in recent years, many providers have made the switch to SLT first in response to the LiGHT trial, which showed 74.2% of patients being drop-free three years after primary SLT treatment.2 SLT has been around for decades and has excellent efficacy and safety, as it can help patients avoid drop therapy or be additive alongside drops to lower IOP. The procedure comes without any serious adverse risks that can be associated with intraocular surgeries.
In many cases, IOP is reduced and/or medications are eliminated. If patients do not require topical therapy after the procedure, we recommend IOP checks at least every six months to monitor for increasing IOP. Medication reduction, in particular, will result in happier patients who are appreciative of not having to deal with eye drops. The duration of effect of SLT is substantial, with most treatment effect lasting two to three years on average. The major benefit of SLT is that the procedure can be repeated, potentially providing years of glaucoma control without dependence on eye drops.3
In the few cases where IOP does not respond to SLT treatment and drops are either not working or not tolerated, then MIGS should be considered. Glaucoma patients who develop cataract and are in need of intraocular lens replacement are also an ideal use-case for MIGS, as a surgical procedure is already needed and the drainage implant or technique is additive to it rather than a primary surgery.
 |
|
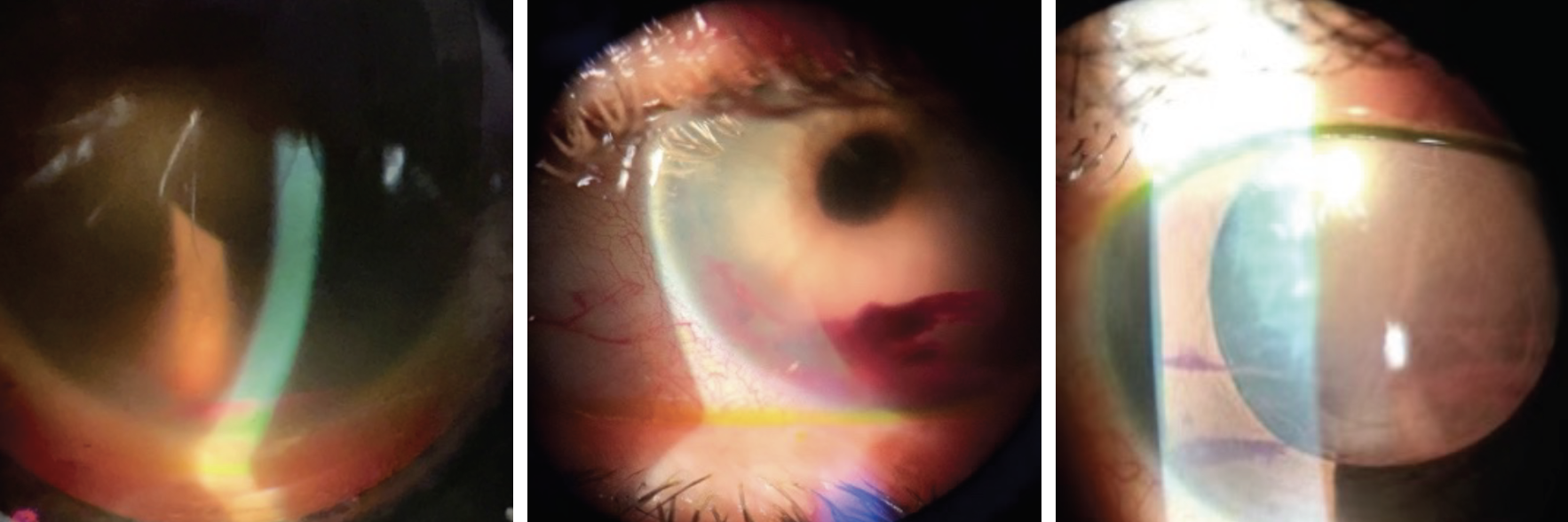
Above are examples of patients with hyphemas post-op day one. Click image to enlarge. |
MIGS
The popularity of MIGS has risen because the traditional surgical options for glaucoma were tube shunts and trabeculectomies. These procedures are wrought with complications, have prolonged healing time and involve large wounds requiring sutures through the conjunctiva. In contrast, MIGS are significantly safer, have a quick recovery time and are sutureless, since they are performed through clear cornea.
Categorizing MIGS can take many different approaches. MIGS is performed as a standalone procedure or in conjunction with cataract surgery; the latter is typically performed when there is phacomorphic component to a patient’s glaucoma or the cataract is visually significant and patient symptomatic. The majority of MIGS are performed via an ab interno approach.
The two main two categories of MIGS are trabecular stents—iStent infinite (Glaukos) and Hydrus Microstent (Alcon)—or trabecular stripping procedures (goniotomy or Omni canaloplasty/trabeculotomy). There is also the Xen Gel Stent (AbbVie), which we place in its own category because it lowers IOP by shunting aqueous fluid to the subconjunctival space.
Below, we will give general recommendations and complications to look out for with these procedures in the postoperative period. It’s important to note that all surgeons have their own protocol. We recommend establishing a good relationship and communicating with your referring surgeon, which will allow you to know each other’s thought processes and preferences for postoperative management, especially if complications arise.
MIGS Options
There are a multitude of options in this category, and their popularity ebbs and flows based on a combination of individual surgeon preference/experience and documented outcomes in the literature influencing uptake. Below, we will limit our discussion to those most popular at our clinic.
Goniotomy or trabeculotomy with canaloplasty (Omni procedure)
Both goniotomy and Omni procedures have been a popular choice by surgeons. I (Dr. Yadgarov) especially like the Omni due to its dual mechanism of canaloplasty and trabeculotomy. You can explain this to patients as a “Roto-rooter” plumbing procedure that helps the drainage of aqueous fluid. The Omni procedure typically works the day following surgery, but if there is inflammation, its full effect may take up to four to six weeks post-surgery.
CPT code: 65820 or 66174 (coordinate with surgeon).
Indication: Open-angle glaucoma of any stage, not controlled on eye drops or not tolerant of eye drops.
Global post-op period: 90 days.
Recommended post-op visits: Day one, week one, month one.
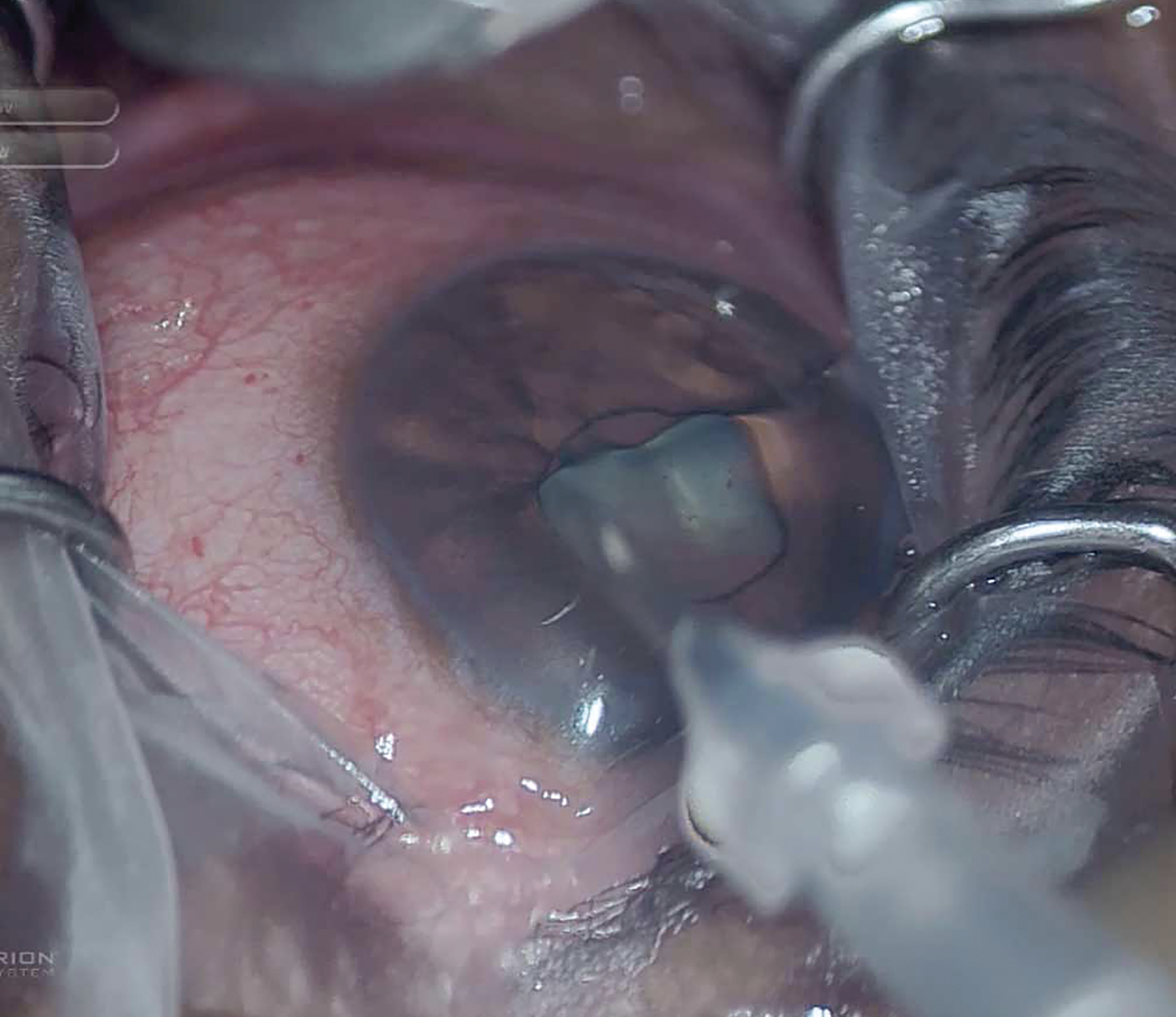
iStent infinite4
This product is the first standalone implantable device for patients with primary open-angle glaucoma and, since its creation, Glaukos has continued to improve upon its design. Surgeons can insert up to three iStents into an auto-injector system approximately six clock hours around Schlemm’s canal. The stents are designed to lower IOP by restoring the natural physiological outflow of aqueous humor.
CPT code: 0671T.
Indication: Open-angle glaucoma of any stage, in patients who have failed prior medical or surgical intervention.
Global post-op period: If performed standalone, there is no global period, so visits after surgery can be billed as office visits. If performed in conjunction with cataract surgery, then standard 90-day post-op is valid.
Recommended post-op visits: Day one, week one, month one.
Hydrus Microstent5
This is by far the largest-sized MIGS option available. The device covers 90° within the angle and bypasses the trabecular meshwork to help outflow via Schlemm’s canal. It can only be inserted during cataract surgery.
CPT code: 66991
Indication: Mild-to-moderate open-angle glaucoma.
Global post-op period: 90-day post-op due to conjunction with cataract surgery.
Recommended post-op visits: Day one, week one, month one.
 |
|
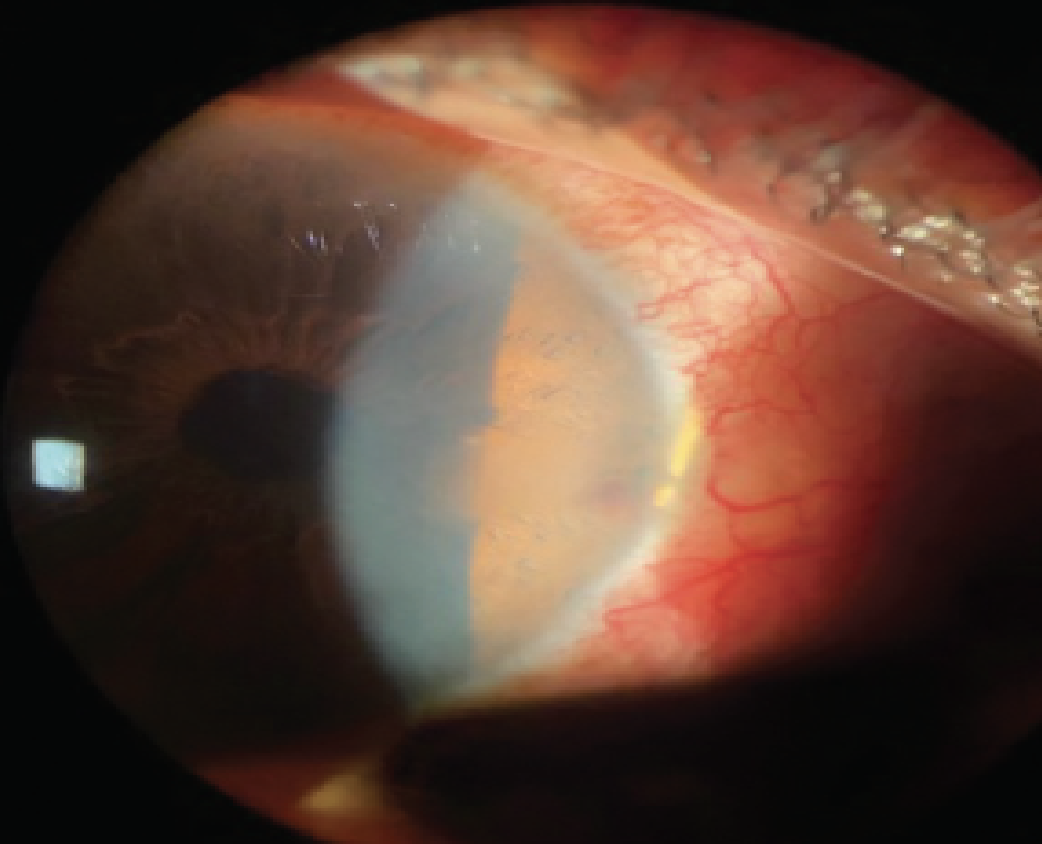
This patient has a more translucent limbus where the Hydrus Microstent is visible on slit lamp within the nasal angle. This should not be a cause for alarm. Of note, observe the significant conjunctival injection and faint hyphema at the stent opening, which warrants a topical steroid to control the inflammation. Photo: Katie Harris, OD. Click image to enlarge. |
Xen Gel Stent6
While some consider the Xen implant to br a MIGS treatment, most doctors have this procedure in its own category due to the mechanism of action and complications that can arise, as well as revisions necessary to maintain function.
CPT code: 66183.
Indication: Refractory glaucoma, including cases where previous surgical treatment has failed, cases of primary open angle glaucoma and pseudoexfoliative or pigmentary glaucoma with open angles that are unresponsive to maximum tolerated medical therapy.
Post-op period: 90 days.
Post-op visits: Day one, week one, week three, then monthly.
 |
|
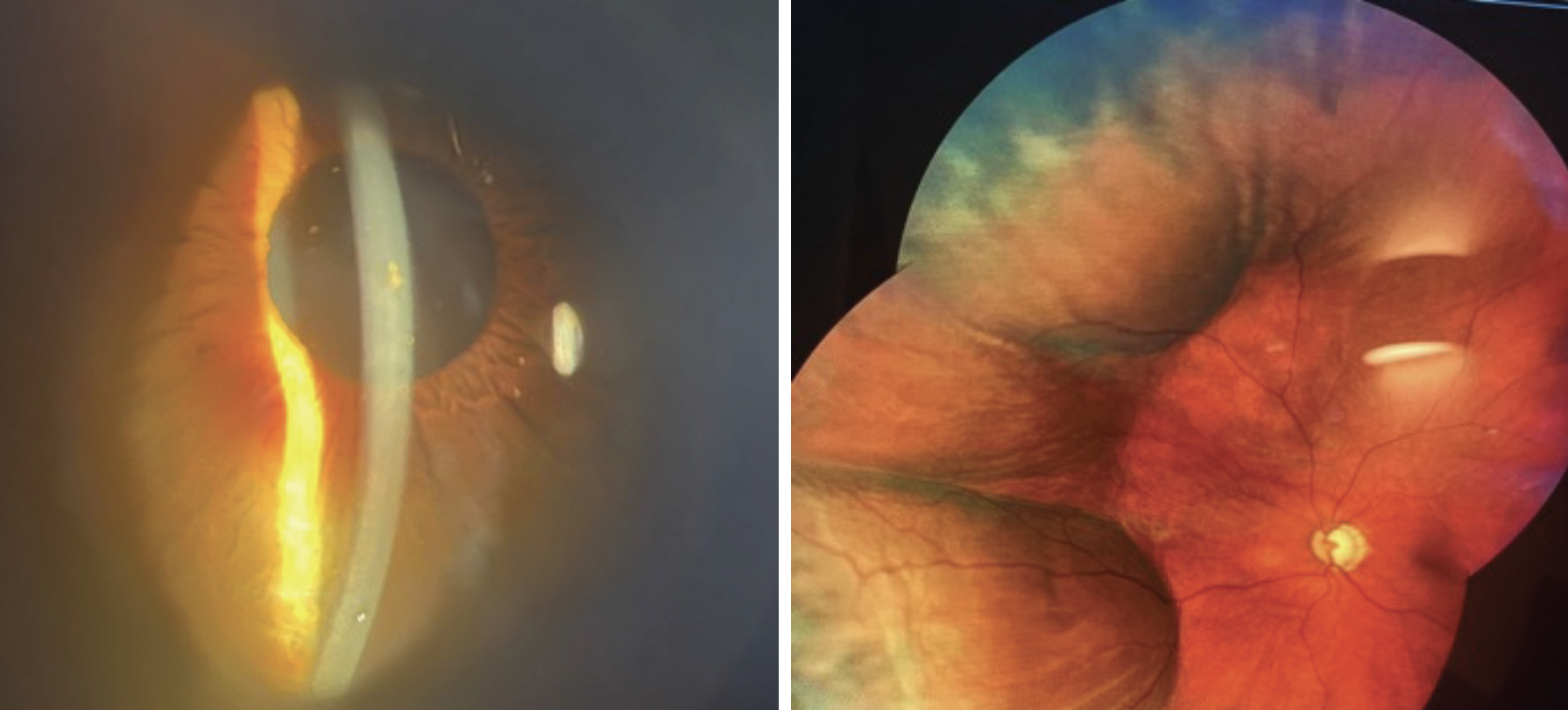
An example of a shallow anterior chamber post-Xen stent in a patient with an IOP of 3mm Hg. Choroidal detachments were confirmed on fundus examination. Click image to enlarge. |
Post-op After Cataract Surgery and MIGS
Adequate IOP reduction can often be unpredictable and treatment effects can wane quickly. Here’s what follow-up visits should consist of:
Day one. Just like a typical cataract surgery patient, this visit consists of a vision and an IOP check. NaFl dye should be instilled to confirm a negative Seidel test. If IOP is elevated on day one, it is either due to retained viscoelastic or a weakened trabecular outflow system. We do not recommend burping the wound unless IOP >40mm Hg (to avoid causing inadvertent hyphema).
For IOP between 21mm Hg and 30mm Hg, we recommend a short course of a single, quick-acting IOP-lowering drop, such as dorzolamide or brimonidine/timolol; there is no harm using a combination drug like these.
For IOP between 30mm Hg and 40mm Hg, we recommend a combination IOP-lowering drops and seeing the patient several days later (before a typical one-week visit). For IOP greater than 40mm Hg, either burp the paracentesis wound or use oral acetazolamide (two 250mg tablets BID) for the first three days along with a combination IOP-lowering drop and see the patient back in two to three days.
Week one. This visit is needed to make sure the patient is healing appropriately as a patient would post-cataract surgery. You also want to check to make sure the IOP is at an appropriate target. We recommend gonioscopy at this visit to confirm the glaucoma stent device inserted during surgery is in good position and open and not obstructed.
Weeks three and four. Depending on previous healing and findings at the previous visit, sometimes patients need to return sooner than one month. This is a good visit to determine how well the IOP is controlled; mild glaucoma patients whose IOPs are controlled and on less or no glaucoma medications can potentially return after the three-month global period to re-establish glaucoma care with new baseline testing.
Month two. For moderate to severe primary open-angle glaucoma patients, we recommend this visit to allow a second IOP check to confirm stability of glaucoma control.
After 90 days. We recommend obtaining updated glaucoma testing to re-establish glaucoma care or establish new baselines if drops were discontinued or reduced.
Postoperative Drops
Broad-spectrum antibiotics QID five days to one week (unless dropless surgery is performed) are recommended, along with topical steroids (again, unless the patient had dropless surgery) and glaucoma drops.
Mild-to-moderate glaucoma patients on one medicine can typically stop their glaucoma medicine one day after surgery. If the patient had been on multiple topical medications, it is recommended to stop one bottle and re-assess IOP after a few weeks of recovery. Our office typically stops the prostaglandin class first due to possible pro-inflammatory characteristics of the drop. If IOP continues to be low, another bottle can be trialed off.
For severe glaucoma patients, we caution to not stop all medicines, as these patients usually have a weakened trabecular outflow system and need MIGS as well as medical therapy to maintain IOP stability. Most severe patients need to stay on at least one medication to maintain a stable and low enough target pressure. However, if the patient is able to discontinue all medications, we recommend IOP checks every three to four months to detect elevating IOP or fluctuations.
Early Complications of MIGS
Postoperative management is more complex than other MIGS procedures due to the risk of complications and need for additional intervention.
Postoperative inflammation. This is more common when cataract surgery is combined with glaucoma procedures. A slit lamp examination can reveal one or more of the following: diffuse or, more commonly, limbal conjunctival injection, cells in the anterior chamber and corneal edema.
In some cases, a topical steroid dosed QID is needed (sometimes Q2H if there is also fibrin or significant pain). Also, the IOP can rise depending on amount of inflammation, but don’t be afraid to use steroids during the inflammatory phase; prednisolone acetate is usually sufficient enough. Difluprednate can also be used dependent of severity if the inflammation seen. Dosing can range from QID to Q2H dependent on severity. Steroid response typically takes many weeks to set in.
Hyphema. This typically occurs with trabecular stripping MIGS procedures such as goniotomy or trabeculotomy (Omni procedure). A slit lamp examination can reveal visible blood on the corneal endothelium or angle. If we do not see an obvious hyphema within the angle on slit lamp, we are highly suspicious of a microhyphema when we see 4+ cells in the anterior chamber on a post day one or week one visit. Gonioscopy can be performed during the week one visit to confirm a small hyphema in the inferior angle or a hyphema along the nasal trabecular meshwork. Postoperative hyphemas usually self-resolve (unless the IOP is persistently high).
We recommend staying on prednisolone three to four times a day until most of hyphema has resolved, which typically takes one to two weeks. If still present, be cautious with steroids, as IOP will start to rise after two weeks of use. After most of the hyphema has resolved, a standard or a quick steroid taper can be initiated. If the IOP rises, start topical medications and see the patient back within two to three days. If the IOP is still high (>21mm Hg) despite escalating treatment, reach out to the surgeon to discuss whether an anterior chamber washout is best.
We also recommend patients sleep at a 45° incline (with an extra pillow under their head at night) to help the blood settle quicker.
Steroid response. This is not a common occurrence, as most patients are tapered off within a month before the steroid response has time to kick in, but it does occur in those who have an inflammatory predisposition. If IOP rises within a few weeks of steroid use, we recommend adding quick-acting combination glaucoma drugs and not stopping the steroid until the anterior chamber cell has substantially resolved, and then tapering. Once the patients is tapered off the steroid, the glaucoma drugs can be trialed off.
We recommend seeing the patient back in a few weeks to make sure the IOP is controlled. If topical medications are not controlling IOP, communicate with the surgeon.
Infection. Postsurgical endophthalmitis is extremely rare. Ensuring there are Seidel negative wounds and that the patient is following proper instructions and wearing an eye shield at night is important.
Malpositioned stents. Occasionally, due to the microinvasive nature of procedure, trabecular stents may not be positioned perfectly into the trabecular meshwork. These stents do not cause any associated ocular issues and can be left in place as long as they are not causing corneal endothelial disruption. A scenario that is typical for a malpositioned stent is when IOP does not lower much despite the MIGS procedure. Gonioscopy after the week one visit can confirm this scenario.
Xen-specific Complications
Hypotony (IOP <6mm Hg) and elevated IOP are two complications patients may experience after implantation of the Xen stent. Hypotony is most commonly experienced and we tend to describe this to the patient as the stent is working “too good.” It’s usually temporary and dilation is needed to detect choroidal detachment. If the anterior chamber is shallow or there are choroidal detachments, starting a cycloplegic agent like atropine and increasing topical steroid tends to help these eyes recover quicker. In some cases, it’s critical to consult a surgeon.
Elevated IOP usually happens due to scarring around the stent. If the IOP is >13mm Hg at any of the visits or IOP is trending upwards, we recommend reaching out to the surgeon to assess if a minor Xen revision is needed with the surgeon to improve Xen stent flow and open the stent back up.
Long-term Complications
 |
|
iStent Infinite has proven to be a safe and effective MIGS procedure to lower IOP and improve aqueous outflow. Click image to enlarge. |
While rare, there are some possible hurdles patients may experience down the road that they need to be aware of.
Best-corrected visual acuity loss. This is a rare but serious complication that can arise in patients with moderate to advanced glaucoma who have field loss close to central fixation or extensive ganglion cell damage preoperatively. Procedures that drop IOP significantly, such as the Xen stent, can occasionally “snuff out” the central vision and result in worsened final visual acuity than what the patient started with. Counseling patients appropriately is imperative to ensure realistic expectations and assess patients’ risk tolerance. To potentially reduce this risk, avoid the Xen stent in eyes with extensive ganglion cell damage—unless IOP is high—in which case, after appropriate counseling and acceptance of risk, surgery is recommended to prevent glaucoma progression.
Endothelial cell loss. Any device inserted within the anterior chamber can potentially cause endothelial cell loss. Both iStent and Hydrus have long-term data that show no significant endothelial cells over two to five years.
Failure of MIGS. No glaucoma treatment is permanent. It is important and prudent that patients understand MIGS or any glaucoma procedure doesn’t last forever and IOP can still rise over time. It is also imperative they understand that even with MIGS and stopping their glaucoma medicines, they still need to show up to clinic at least twice a year (more often dependent on glaucoma severity) to have their glaucoma monitored. If IOP does rise over time, despite MIGS, eye drops may need to be restarted to avoid the chance of glaucoma progression.
Takeaways
The optometric profession has evolved from the early days of a “glasses-only” specialty, as many states now allow ODs to provide more advanced medical care, including minor surgical procedures. With all of these expansions, one of the most powerful advantages optometrists have is the ability to maintain care of their own patients by performing postoperative care. Glaucoma, in particular, is undergoing an interventional renaissance and partnering with your local glaucoma specialist will greatly benefit your patients. MIGS postoperative care is a critical element in a patient’s glaucoma journey, and we encourage each of you to be a part of that experience.
Dr. Love received her doctorate in Optometry from the University of Alabama at Birmingham and completed her ocular disease residency at Omni Eye Services of Atlanta. She has worked at Ophthalmic Consultants of Connecticut, Omni Eye Services of Atlanta and served as clinical director for TLC Laser Eye Centers in Fairfield, CT. Dr. Love has represented the American Board of Optometry as an ambassador in Connecticut and currently in Georgia. She is a consultant for Dompé. Dr. Yadgarov is a board-certified ophthalmologist who graduated summa cum laude from Georgia Tech and received his MD degree from the Medical College of Georgia. He completed his ophthalmology residency at the Institute of Ophthalmology and Visual Science of Rutgers University. He then completed his glaucoma fellowship at the New York Eye and Ear Infirmary. Dr. Yadgarov currently practices at Omni Eye Services of Atlanta, where he performs cataract surgery and provides glaucoma care with a special interest in minimally invasive glaucoma surgery. He is a member of the American Academy of Ophthalmology, American Society of Cataract and Refractive Surgery and the American Glaucoma Society. Dr. Yadgarov is a consultant for Alcon, Glaukos and SightSciences.
1. Law SK. First-line treatment for elevated intraocular pressure (IOP) associated with open-angle glaucoma or ocular hypertension: focus on bimatoprost. Clin Ophthalmol. 2007;1(3):225-32. 2. Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicenter randomized controlled trial. Lancet. 2019;393(10180):1505-16. 3. Realini T, Shillingford-Ricketts H, Burt D, Balasubramani GK. Long-term outcomes of selective laser trabeculoplasty for open-angle glaucoma in the Caribbean. Am J Ophthalmol. 2021;232:83-9. 4. iStent infinite. www.glaukos.com/glaucoma/products/istent-infinite/. Accessed June 25, 2024. 5. Hydrus. www.myalcon.com/professional/cataract-surgery/hydrus-microstent/. Accessed June 25, 2024. 6. Xen. hcp.xengelstent.com/content/dam/xengelstenthcp/pdf/dfu_xen_glaucoma_treatment_system_us_feb2017.pdf. Accessed June 25, 2024. |

