 |
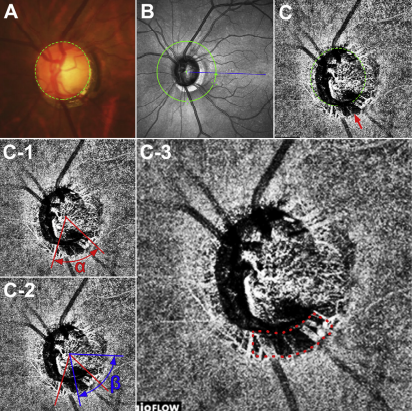
| Patients with higher mean rates of change in the choroidal microvasculature dropout area may be at an increased risk of accelerated vision loss. Photo: Vaishaali Gunalan, M. Optom. Click images to enlarge. |
Authors of a recent study discovered a structure on OCT that may help to identify glaucoma patients at greater risk of more rapid visual field loss: microvasculature dropout (MvD). In the study cohort, MvD area rates were associated with visual field loss in patients with primary open-angle glaucoma (POAG). Conversely, when the team looked at beta-zone parapapillary atrophy (β-PPA) area rates, they found no association with visual field loss among this patient population.
The retrospective, observational cohort study involved 76 eyes from 58 POAG patients with and without localized MvD who attended a tertiary glaucoma clinic. All patients had at least two years of follow-up and a minimum of four visits of OCT-A and OCT scans. The researchers evaluated a total of 468 scans and calculated rates of MvD change, β-PPA area change and visual field mean deviation change.
The mean rates of MvD and β-PPA area change were 0.039mm2 and 0.037mm2 per year, respectively, throughout the four-year follow-up. Enlargement of MvD area was significantly associated with faster rates of visual field mean deviation loss (0.03mm2 per 1dB worse), though the same was not true for β-PPA area enlargement (0.04mm2 per 1dB worse).
“Recent studies have shown that MvD has increased in size for some individuals with glaucoma,” the researchers wrote in their study, published recently in the American Journal of Ophthalmology. “Hence, it has been proposed that the extent of the enlargement is associated with faster glaucoma progression, a result confirmed by our study.” They add that “there exists a notable topographic correspondence between MvD and RNFL defects, both in terms of location and extent, which suggests that MvD exhibits a stronger association with glaucoma than β-PPA does.”
The researchers propose a few other explanations for why the rate of β-PPA area change didn’t appear to have an association with visual field loss in this study. “There is still debate about whether PPA is a consequence of glaucomatous optic neuropathy or if it is a contributing factor,” they wrote in their paper. “It is also unclear whether PPA is present before the onset of glaucoma and predisposes the eye to glaucomatous optic neuropathy or if it develops later in association with glaucoma and progresses along with glaucomatous optic neuropathy.” They go on to cite the conflicting findings of several studies that ultimately suggest a lack of robustness in the association between β-PPA and glaucoma.
In summary, the study authors conclude that MvD is an independent predictor of accelerated visual field loss in glaucoma patients, and its rate of enlargement has a greater ability than β-PPA change to identify those at risk for rapid vision loss.
Latif K, Nishida T, Moghimi S, Micheletti E, Du K, Weinreb RN. Relationship of choroidal microvasculature dropout and beta-zone parapapillary area with visual field changes in glaucoma. Am J Ophthalmol. August 11, 2023. [Epub ahead of print]. |

