 |
|
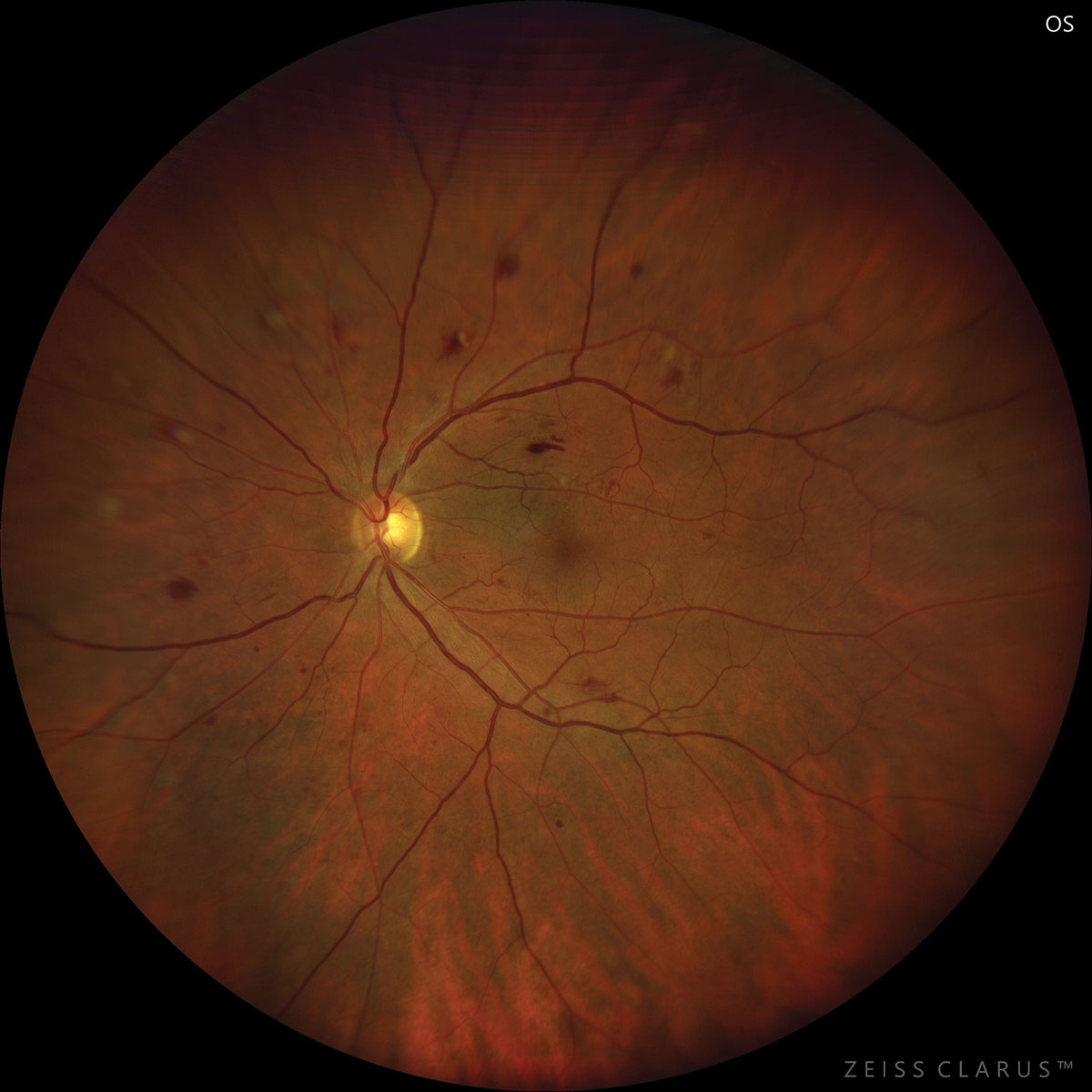
The advent of newer oral hypoglycemic agents for reducing blood sugar levels in those with diabetes has raised the awareness of their effects on the risks and progression of diabetic complications, including diabetic retinopathy (DR). A recent meta-analysis specifically reviewed real-world results of dipeptidyl peptidase-4 inhibitor use and found no significant risk or progression of DR, although larger population studies are warranted. Photo: Jay Haynie, OD. Click image to enlarge. |
Good glycemic control is paramount in the management of diabetes mellitus (DM), which in turn helps reduce the risk and progression of micro- and macrovascular complications, including diabetic retinopathy (DR). Oral hypoglycemic agents are one tool in the toolbox for diabetes patients with DM, of which sulfonylureas and metformin have long been the first-line therapy. However, the advent of newer drugs, including dipeptidyl peptidase-4 inhibitor (DPP4i), and the limited data available for them, calls into question their true impact on diabetic complications. A recently published meta-analysis says there is no real-world evidence that DPP4i affects the incidence and progression of DR.
Researchers did a deep dive into seven cohort studies published up to July 2023 using databases from PubMed, Central, Embase, Scopus and Web of Science. Four studies reported data on the incidence of DR with the use of DPP4i, and a meta-analysis showed that it wasn’t associated with any significant change in DR risk; and three studies on the progression of DR with the use of DPP4i also showed no significant risk of DR progression, after a meta-analysis.
Although this was the big picture, a closer look at the individual studies show conflicting results, noted the study authors. In regards to the lack of impact on DR progression, the authors said one small study showed a reduced risk, while a large study demonstrated an increased risk, and yet another study found no effect. The authors of this study hypothesized that the differences in study populations and the method of assessing DR progression, such as ICD codes or a validated scale, could have led to variable results.
Given the current data, the true effects of DPP4i on the retina are unclear. “Clinically, a number of factors could explain such variations as the duration of diabetes, baseline glycemic control, use of other hypoglycemic agents, duration of therapy, etc.,” wrote the authors. While randomized controlled trials have a low risk of bias due to the predefined inclusion criteria, blinding and the prospective nature of the research, they explained, “the study population tends to be restrictive and may not reflect the complex scenario seen in the real world.”
One drawback of this review is the observational nature of the data used in the studies, derived from medical records. “The possibility of selection bias in the prescription of drugs cannot be ruled out,” statedd the authors. “Duration and compliance of drug therapy cannot be firmly confirmed as data is derived mostly from pharmacy records,” the paper notes “Diagnosis of DR and its progression was not clinical and was sourced from medical records or the requirement of intervention for DR. Such a definition may not be completely inclusive of patients with DR progression.”
The study authors also mentioned the important confounders involved in DR risk, including older age, duration of DM, hypertension, glucose levels and lipid drugs, among other diabetic microvascular complications. These could have been missed in some of the studies, which could have affected outcomes.
Real-world studies on DPP4i are limited, but seem to convey that the drug doesn’t significantly influence the incidence and progression of DR, but further studies from other countries with accurate definitions of DR are needed to validate the current results, concluded the authors.
Wang M, Lu J, Dong J. Association between dipeptidyl peptidase-4 inhibitor use and diabetic retinopathy: A systematic review and meta-analysis of real-world studies. BMC Ophthalmology. June 28, 2024. [Epub ahead of print.] |

