 |
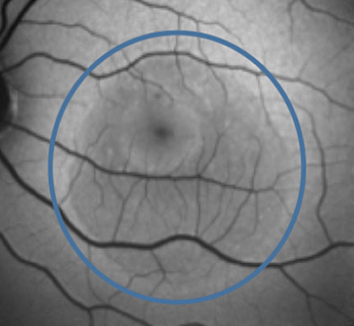
Outcome analysis revealed that history of steroid use was associated with a decreased need for CSCR treatment and better final visual acuity; eyes with lower baseline best-corrected visual acuity were associated with increased need for treatment and worse final visual acuity. Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
Some patients with central serous chorioretinopathy (CSCR) tend to develop a chronic form of the disease, which if untreated, results in a recurrent/persistent course, or the patients develop choroidal neovascular membrane that can lead to permanent vision loss. A newly validated multimodal imaging-based CSCR classification allows doctors to categorize the disease based on severity and prognosis. The team thought it was pertinent to understand the gender-specific associations using this new system and analyze long-term changes in male and female patients. They found that males tended to have complex CSCR recurrence and progressive decline in vision, while females exhibited choroidal neovascularization more commonly.
The study included 109 eyes of 58 patients (55 eyes of 28 female patients and 54 eyes of 30 male patients). The term “simple” was used for eyes with retinal pigment epithelium alterations of less than/equal to two disc areas, and the term “complex” was reserved for eyes with more than two disc areas or multifocal retinal pigment epithelial alterations.
Simple CSCR was seen in eight (14.8%) eyes and 21 (38.2%) eyes in male and female groups respectively, while complex CSCR was seen in 46 (85.2%) eyes and 34 (61.8%) eyes in male and female groups respectively. Recurrence was more commonly seen in males (34 eyes) than in females (23 eyes). Males (96.7%) were also significantly more likely to have a bilateral presentation (78.6% in females). Conversely, choroidal neovascularization was more commonly seen in female eyes (eight eyes) than male eyes (four eyes).
The researchers did not find any significant effect of gender on the need for treatment and final visual acuity. On multivariable regression analysis, factors affecting reduced need for treatment were history of steroid use, good visual acuity at baseline and simple CSCR. Factors affecting good final visual acuity were history of steroid use, good visual acuity at baseline and younger age.
“It is yet to be determined if there is change in these characteristics over the long-term, or if there is any genetic susceptibility justifying this difference, for which larger, more controlled, prospective studies will be required,” the researchers concluded in their paper.
Sahoo NK, Ong J, Selvam A, et al. Gender differences in central serous chorioretinopathy based on the new multimodal imaging classification. Eye (Lond). November 4, 2023. [Epub ahead of print]. |

