There is no infallible biomarker for glaucoma, particularly early in its course. It remains a clinical diagnosis based on the demonstration of distinctive structural and functional changes, which can lead to uncertainty in the early stages when some but not all features are present. Optic disc appearance and automated perimetry are often used to detect glaucoma and to predict development of the disease. Could electrophysiological testing give clinicians an early indication, especially during the pre-perimetric phase of the disease when field loss has yet to develop?
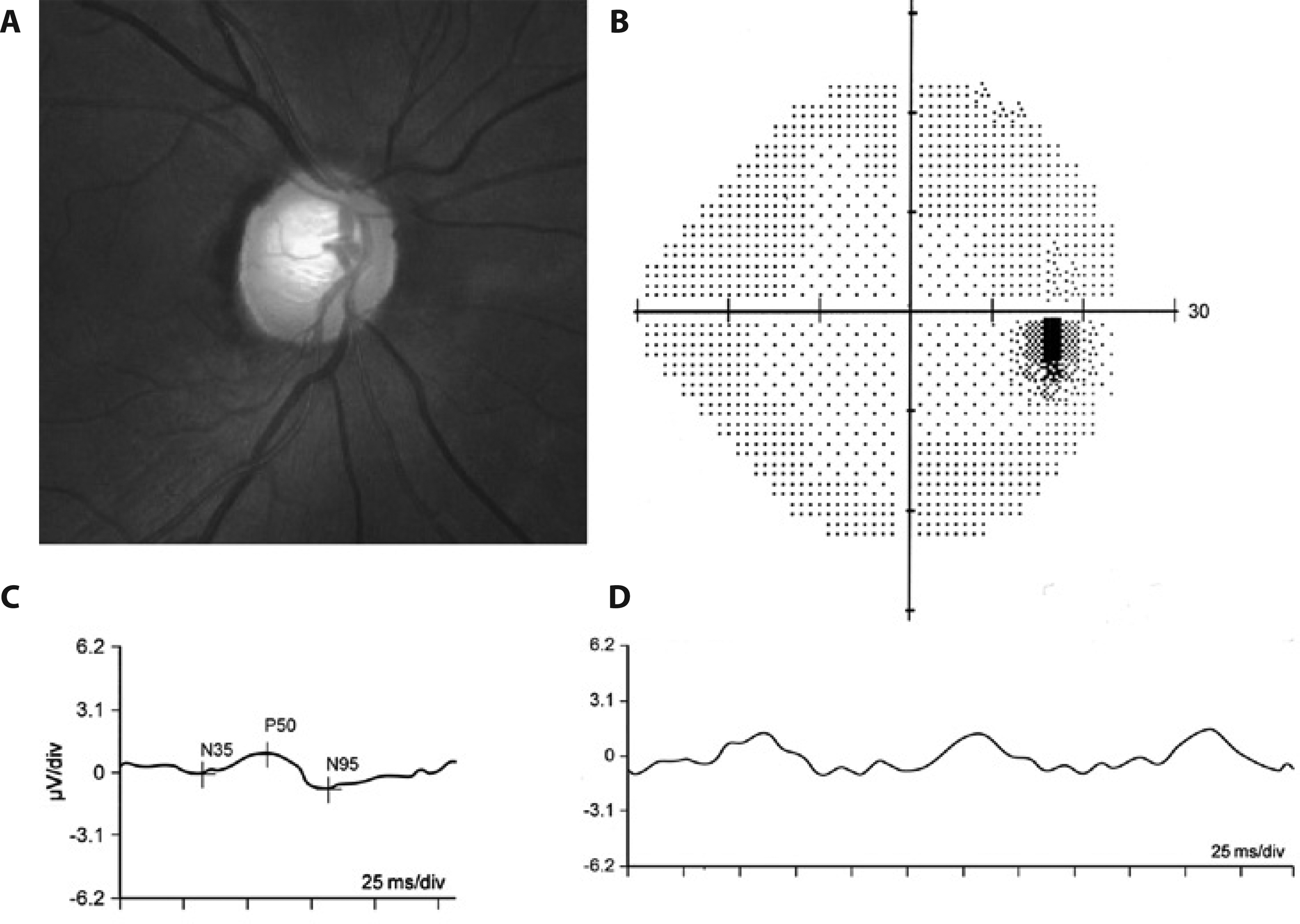 |
| Representative example of an eye with pre-perimetric glaucoma and reduced pERG responses: (a) Fundus photo showing glaucomatous cupping; (b) normal 24-2 SITA Standard visual field result; (c) reduced transient pERG responses (P50 = 0.95μV; N95 = 1.65μV); (d) reduced steady-state PERG amplitude response (1.78μV). Photo: Kreuz AC. Arq. Bras. Oftalmol. 77(6), Nov-Dec 2014. Click image to enlarge. |
Researchers in Bavaria, Germany recently conducted a retrospective, longitudinal cohort study with a very long follow-up to study whether pattern electroretinograms (pERG) amplitudes and blue-on-yellow visual evoked potential (VEP) latencies could predict visual field (VF) defects. They found that lower pERG amplitudes were associated with increased risk of development of visual field defects, independent of optic disc changes. The team believes that electrophysiological parameters such as pERG amplitude could potentially increase the value of multifactorial models for predicting the risk of conversion to perimetric glaucoma in patients at risk.
Their study tested 412 patients (70% with normal optic discs, 25% with enlarged cups but no focal notch, 5% with temporal notching; baseline age: 20 to 60 years) using pERG and blue-on-yellow VEP. Patients were treated according to clinical standards and performed standard automated perimetry annually. Retrospectively, patients with normal fields at baseline were selected. Primary endpoint was conversion to perimetric glaucoma.
Of 412 patients, 15.8% converted to perimetric glaucoma during follow-up. Optic disc classification was a strong risk factor for conversion, and patients with more advanced changes progressed earlier. Patients with more advanced neuroretinal rim loss progressed much earlier than those with normal neuroretinal rim, even when under treatment according to standard clinical practices. The small subgroup with notching at baseline had a median time to conversion of 5.1 years vs. 15.3 years for those with enlarged cups; in patients unaffected at baseline, even the 25% conversion rate was >22 years.
In the multivariate analysis, only pERG amplitude remained an independent risk factor after stratification for optic disc morphology, with an about 30% higher risk per μV amplitude decrease.
In their paper, the researchers wrote that they believe that “pERG allows demonstration of dysfunction in viable ganglion cells.” However, they did note that “the fact that morphological classification [of the optic nerve head] is much more easily available in clinical practice means that the electrophysiological markers only have a value if they yield additional information for predicting progression.”
They also pointed out that OCT measurement of RNFL and retinal ganglion cell layer thickness were not available when baseline measurements were performed, as the study began recruiting patients as early as 1991. “We cannot rule out that these tools would have demonstrated more subtle structural changes that yield the same information as the PERG amplitudes.”
Huchzermeyer C, Lämmer R, Mardin CY, et al. Pattern electroretinogram, blue-yellow visual evoked potentials and the risk of developing visual field defects in glaucoma suspects: a longitudinal "survival" analysis with a very long follow-up. Graefes Arch Clin Exp Ophthalmol. January 6, 2024. [Epub ahead of print]. |

