 |
A 57-year-old Hispanic female presented with symptoms of seeing occasional purple spots in her vision for the past three weeks. She was not sure if this was limited to one eye. Beyond that, she stated her vision was good and that she only wore reading glasses.
Her medical history was significant for Type 2 diabetes and a recent HIV diagnosis. She was taking medications but did not know their names, nor did she know her CD4 count or her viral load.
Her best-corrected visual acuity was 20/20 OU. Confrontation visual fields were full-to-careful finger counting. The pupils were equally round and reactive; no afferent pupillary defect was seen. The anterior segment was unremarkable in both eyes. There were trace cells in the anterior vitreous in the right eye. The left eye was clear. Tensions by applanation measured 11mm Hg OU.
The optic nerves appeared healthy with small cups and good rim coloration and perfusion. We noted obvious retinal findings in both eyes (Figures 1 and 2).
Take the Retina Quiz
1. What do the peripheral retinal changes in the right eye represent?
a. Retinal vein occlusion.
b. Active chorioretinitis.
c. Active retinitis.
d. Inactive retinitis.
2. What do the white spots in the posterior pole represent?
a. Cotton wool spots.
b. Drusen.
c. Exudate.
d. Roth spots.
3. What is the diagnosis?
a. Toxoplasmosis.
b. Acute retinal necrosis.
c. Cytomegalovirus retinitis.
d. Proliferative diabetic retinopathy.
4. How should this patient be treated?
a. Observation.
b. Anti-VEGF injection.
c. Begin anti-viral therapy.
d. Begin antibiotic therapy.
For answers, see below.
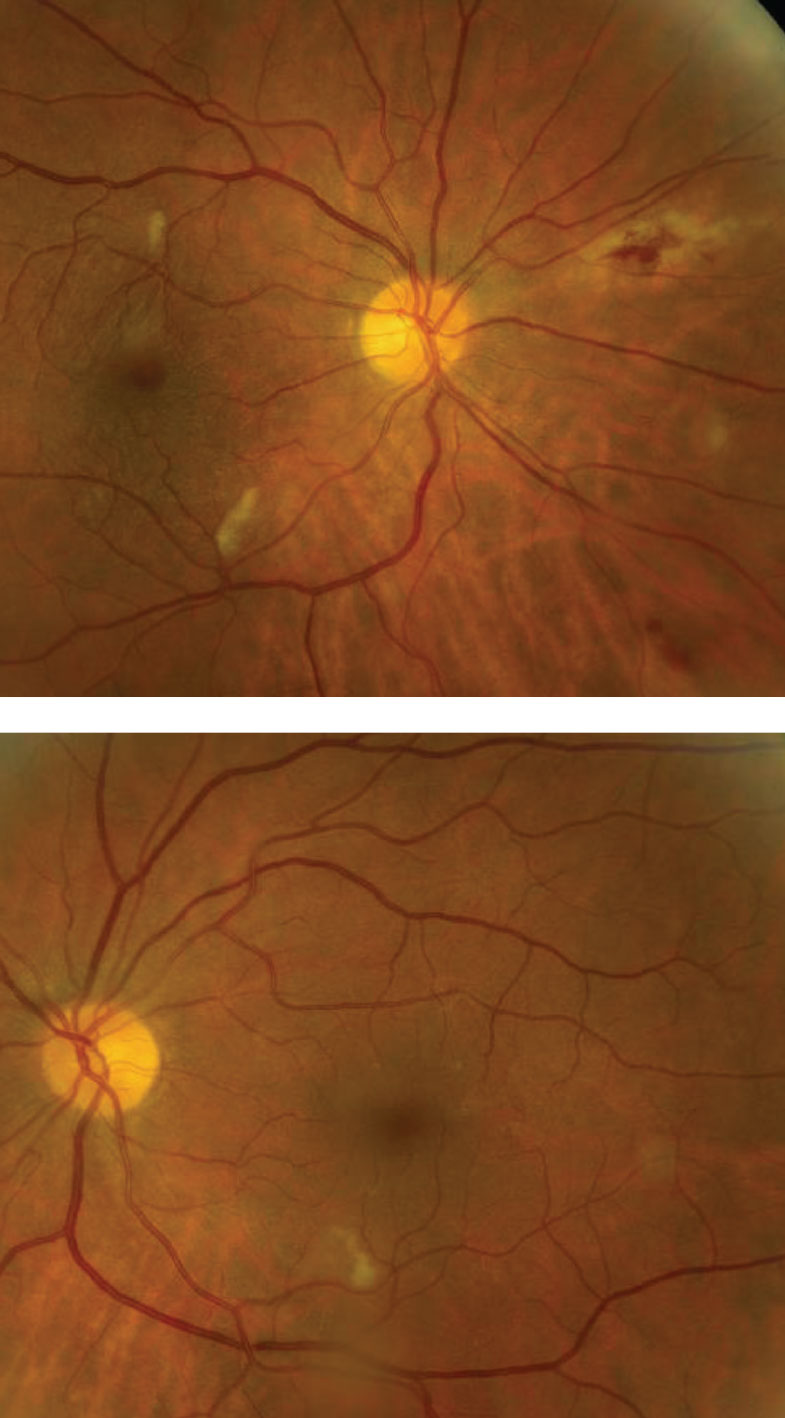 |
| Figs. 1 and 2. Note the peripheral retinal changes nasally in the right eye (above). Can you identify the finding in the posterior poles of both eyes? Click image to enlarge. |
Diagnosis
The nasal peripheral retinal changes in the right eye represents active cytomegalovirus (CMV) retinitis. CMV is one of the herpes viruses that infects most adults.1 Almost all of us have been exposed to CMV in our lifetime but will have no symptoms of infection because our immune system is strong enough to keep the virus in check.1 But, in people with weakened immune systems, like our HIV patient, the virus can reactivate and spread to the retina, which can lead to vision-threatening complications.1
CMV retinitis is the most common ocular complication seen in patients with HIV.1 CMV retinitis develops in patients whose CD4+ lymphocyte T-Cell (CD4) counts are below 50 and usually even much lower than that. With the advent of highly active antiretroviral therapy (HAART), CMV has virtually disappeared, with a dramatic 55% to 95% decline in the number of CMV retinitis cases.1
Discussion
CMV retinitis may be present anywhere in the retina.1 Posterior pole lesions have a characteristic white, hemorrhagic appearance with retinal necrosis and edema, while the peripheral lesions are more indolent and nonhemorrhagic.1 The active retinitis generally follows the path of the retinal vasculature centripetally.1 In rare instances, CMV can also present as a frosted-branch angiitis in which there is a fulminant retinal vasculitis and periphlebitis, giving the fundus a frosted quality to the perivascular exudate.1
Vitreous cells will be present in active CMV but not nearly to the extent seen in, for example, patients with active toxoplasmosis where the vitritis can be so dense the active retinal lesion can be difficult to observe, giving it a “head lights in the fog” appearance.1,2 In contrast, patients with CMV do not have a robust immune system so they are not able to mount a significant immune response; therefore, the vitreous inflammation is minimal and the retinitis can be easily seen.1
What about the white lesions in the posterior pole of each eye; is that CMV retinitis too? Luckily they’re not CMV but rather cotton-wool spots (CWS), which can easily be mistaken for early CMV. The CWS are smaller than CMV lesions and vitreous inflammation will not be present. CWS and even retinal hemorrhages are commonly seen in severely immunocompromised patients with HIV.2 In fact, CWS and retinal hemorrhages are part of the spectrum of HIV retinopathy.2 Though the etiology is not completely understood, researchers say immunocompromised patients have increased plasma viscosity that results in immune-complex deposition.2 This is thought to occur from a direct cytopathic effect of the virus on the vascular endothelium.2
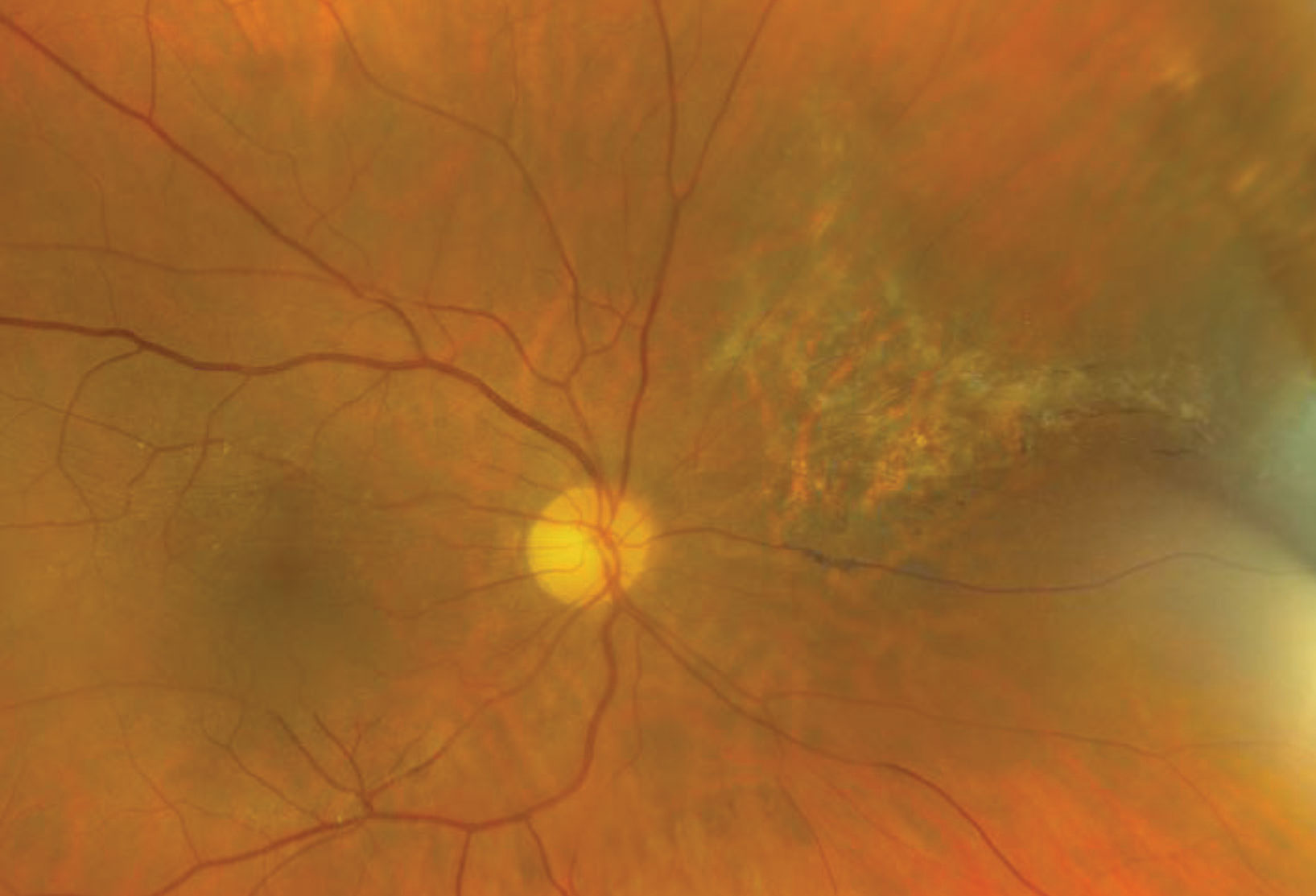 |
| Fig. 3. Here is our patient’s retina five years after initial diagnosis. Click image to enlarge. |
Therapeutic Options
Treatment for CMV retinitis has become fairly standardized with the advent of anti-viral medications including ganciclovir, foscarnet, valganciclovir and cidofovir. Treatment delivery methods include intravenous infusion, oral therapy, intravitreous injection and ganciclovir intraocular implant.3 Specific anti-CMV treatment is individualized for each patient based on the location and severity of the retinitis, level of underlying immune suppression, concomitant medications and ability to comply with treatment.3 Therapy is induced at high doses for two to three weeks or until the retinitis stabilizes followed by a maintenance dose.3 Improved patient survival with HAART has resulted in a paradigm shift away from short-term disease suppression in the early days of treatment to now discontinuation of anti-viral therapy once immune recovery is achieved.3
Clearly, our patient is severely immunocompromised. She did not know her CD4 and had only been recently diagnosed after a bout with pneumonia. She had an immediate intravitreal injection of ganciclovir and subsequently had multiple ganciclovir implants over several years. Eventually, her immune system recovered enough that she was able to discontinue anti-viral therapy for the CMV. She was able to maintain excellent visual acuity in both eyes and we continue to follow her on an annual basis (Figure 3).
1. Jabs DA, Van Natta ML, Kempen J, et al. Characteristics of patients with cytomegalovirus retinitis in the era of highly active antiretroviral therapy. Am J Ophthalmol. 2002;133:48-61. 2. Freeman WR, Chen A, Henderly DE, et al. Prevalence and significant of acquired immunodeficiency syndrome-related retinal microvasculopathy. Am J Ophthalmol. 1989;107(3):229-35. 3. Stewart MW. Optimal management of cytomegalovirus retinitis in patients with AIDS. Clin Ophthalmol. 2010:4;285-99. |
Retina Quiz Answers:
1) c; 2) a; 3) c; 4) c.

