 |
Data! It all comes down to data. The decision of whether to begin treatment for glaucoma depends on visual fields, OCT, intraocular pressures, nerve appearance, family history, expected patient compliance and more. The decision of whether or not to fit a keratoconic cornea with a specific lens design depends on the refraction, topography, visual acuity, available lens materials and a host of other concerns. The decision to refer to a specialist is based on the accumulation of data as well.
So, why should determining a lens prescription be any different? Why should one finding alone be all that is used? The answer: it shouldn’t.
The More the Merrier
In a recent online discussion, a clinician posted patient data with a fairly high hyperopic astigmatism correction and asked for opinions on an appropriate prescription to give the child. There was a decent amount of data provided on which to form an opinion in this case. I (Dr. Taub) typically let these questions go, but I jumped into the fray after seeing the same response a few times: prescribe the entire cycloplegic and nothing less. A lightbulb went off in my head; why would we base the entire endpoint of the examination—in this case, glasses—on one data point?
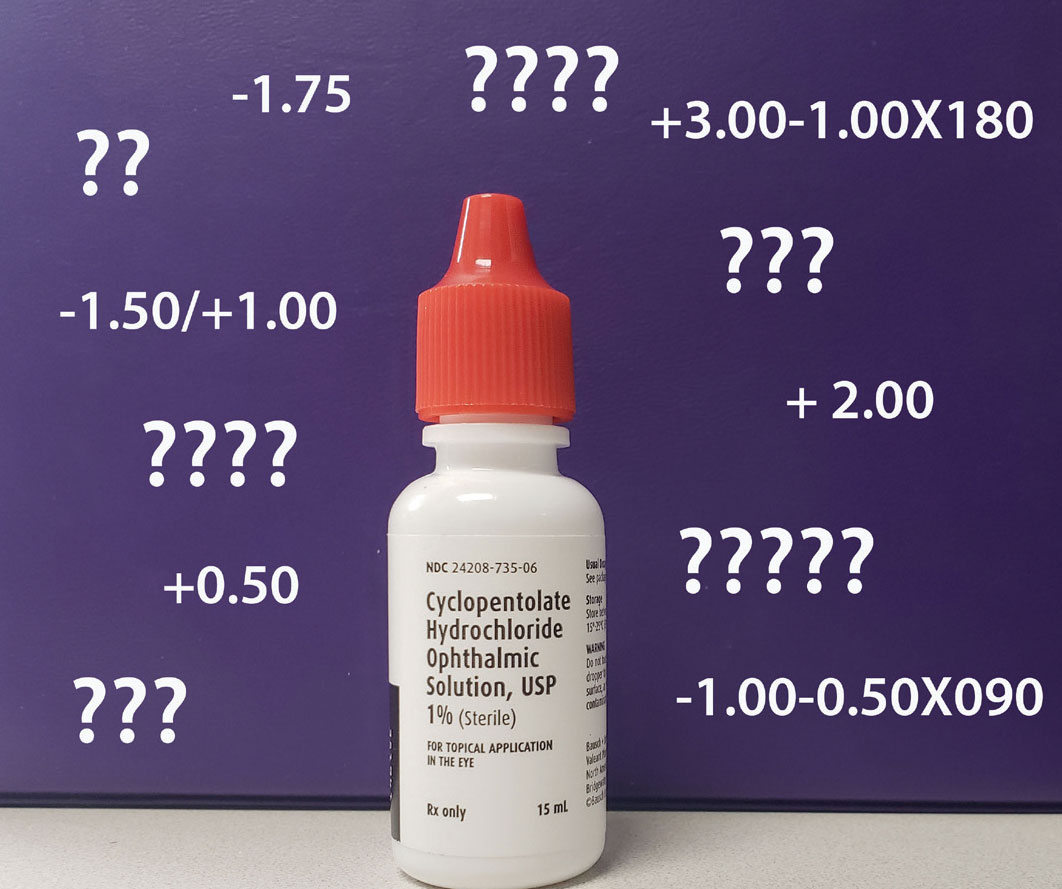 |
| Cycloplegia is effective in evaluating pediatric patients and quantifying refractive error but this finding needs to be balanced against other sources of data before determining an approach to visual correction. Click image to enlarge. |
Over the past six years of this column, we have introduced many aspects for potential use in the clinical examination. We have discussed several data points on which to base the success of a near vision plus prescription, including the MEM, Groffman visual tracing and NPC. We have talked about the Van Orden star, NRA/PRA, retinoscopy at distance and near and different methods for assessing visual acuity. We have presented cases in which the prescription was “cut” to provide better comfort and binocular vision. So, why do so many of us jump at the concept that we must prescribe the full cycloplegic and nothing but the cycloplegic? Why does that data point, of the many we gather, seem to rule over all the others like the one Ring of Mordor?
Perhaps the American Optometric Association’s Evidence-based Clinical Practice Guidelines on Comprehensive Pediatric Eye and Vision Examination can point us in the right direction.1 Released in 2017, it includes over 250 references. In the refraction component of the vision testing sections for both pre-school and school-aged children, the following is stated, “…the results of a refraction do not provide all of the information needed to determine an optical prescription. The refractive error measurement should be analyzed with other testing data and the patient’s visual needs obtained during the in-person examination. This information is used to determine if, and in what amount, an optical correction is needed to provide optimal vision and comfort for all viewing distances.”
There are several things that stand out in this statement:
(1) The refraction is a piece of the puzzle, not the most or only important piece. Going further into the binocular vision, ocular motility and accommodation component of the guidelines, the document specifically encourages examining all of the data without relying on a single finding to make a diagnosis.
(2) The data, whether by static distance retinoscopy, cycloplegic retinoscopy, autorefraction or subjective refraction, does not stand alone and must be considered with all of the other data, including the patient’s history and visual needs.
(3) The piece of data collected should be used to figure out if correction is needed and to help in determining an appropriate amount that provides good vision and comfort.
Perhaps it is time to tackle the concept of balancing optimal vision and comfort head on. Over the years, on a fairly regular basis we have seen children with a need for significant refraction correction return for an appointment either without their glasses or with them in their mother’s purse. When questioned why, typically the response is that the glasses don’t work well, make things worse or feel funny when in use. When we examine the correction, it is usually inevitably high in some manner and an amount that was fully given or based on a cycloplegic refraction, showing the supposed “true prescription.” When the strength is reduced and trial framed, we see similar visual acuity, a more efficient visual system and improved comfort. This harkens back to the concept of prescribing using all of the data points collected and not just one. This concept must be at the forefront of all cases.
So, what does the concept of the true prescription that everyone pulls out of the air in defense of giving every 0.25D found with cycloplegia really tell us? We should start by admitting that many factors get in the way of determining a refractive endpoint, including accommodation, binocular vision and ocular motility. So, when we use cycloplegia, is our goal to determine the true endpoint devoid of, well, all of the other aspects of vision? If our goal is to determine the most appropriate prescription for the visual system, we must examine part of it with all of the noise in the system still present. This is how the patient functions in their everyday lives outside of the optometrist’s office. Does the cardiologist or orthopedist immobilize the heart and knee, respectively, to take measurements? Seems like an odd question but makes for a great analogy.
Another argument for providing the full cycloplegic amount is that we don’t want to leave the patient amblyopic. In looking at the American Optometric Association’s Clinical Practice Guidelines on Amblyopia, revised in 2004, we see that the organization lists the following as amblyogenic factors: isometropia-astigmatism >2.50D, hyperopia >5.00D, myopia >8.00D and anisometropia-astigmatism >1.50D, hyperopia >1.00D, myopia >3.00D and anisometropia.2 So, if the cycloplegic endpoint is determined to be 7.00D OU, you are well within the factor limit if you prescribe only half, or 3.50D. If the prescription shows anisometropia, as long as you reduce the correction within the amblyogenic factor limits, there is no reason to worry about leaving the patient amblyopic or even causing amblyopia in the first place.
Yet another point of discussion is the need to force the patient to wear the full power determined from the cycloplegic. We have seen online posts and had discussions with colleagues in which they state that they make their patients suffer for weeks so that they adapt. Could you imagine an orthodontist saying the same thing? In advertisements for online teeth straightening, they send you a kit of about 20 variations of molds to help guide the process; they don’t just send the final one and say, “suck it up.”
In prescribing, we must accept the concept that it is a process and a negotiation between the doctor, patient and surrounding world in which we live. It is perfectly acceptable to give less than the highest values found to aid in the process of wearing glasses and adapting to them, and then revisiting the prescription at a later date. The prescription will impact the patient and visual system in many ways, so let the patient be part of the process.
Going a little further into the American Optometric Association’s guidelines, the committee states, “There is a lack of published research to support or refute the use of this recommendation.”1 The recommendation, by consensus of the committee members, is that cycloplegia is the preferred procedure for evaluating children and that it is necessary to quantify significant refractive error in the presence of visual conditions such as strabismus, amblyopia and anisometropia.
We find “necessary” to be a very strong word in this case and have not found this to be true, or the consensus of optometrists who see children and provide vision therapy services. Can cycloplegia “enhance the ability to evaluate and diagnose eye and vision problems” as the committee suggests? Yes, but the committee stops short of saying that it is the most important data point.
Takeaways
We have all been taught how the visual system works and how we must weigh all of our examination data to determine the correct diagnosis and appropriate treatment. Being beholden to one data point goes against that concept.
Collect any data that you want, just be aware of how it all comes together to aid in your decision-making process and, ultimately, the treatment you provide.
Dr. Taub is a professor, chief of the Vision Therapy and Rehabilitation service and co-supervisor of the Vision Therapy and Pediatrics residency at Southern College of Optometry (SCO) in Memphis. He specializes in vision therapy, pediatrics and brain injury.
Dr. Harris is also a professor at SCO. Previously, he was in private practice in Baltimore for 30 years. His interests are in behavioral vision care, vision therapy, pediatrics, brain injury and electrodiagnostics. They have no financial interests to disclose.
1. Comprehensive pediatric eye and vision examination. AOA Evidence-Based Clinical Practice Guideline. February 12, 2017. www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/EBO%20Guidelines/Comprehensive%20Pediatric%20Eye%20and%20Vision%20Exam.pdf. Accessed November 10, 2021. |

