 |
When we are called to see patients at a rehabilitation facility, and occasionally when patients are scheduled for vision therapy evaluations at Southern College of Optometry, we truly do not know what we are going to encounter. Brain injury cases range from visual field and acuity loss to visual inattention to vague complaints that something simply “feels off.” Of course, some patients are in such a state of decreased mental and physical capacity that they cannot respond in a traditional manner. Those are the most challenging, but can reap huge rewards for the patients in the long run.
Perhaps the most common complaint we encounter is double vision. This occurs for a multitude of reasons, including muscle and nerve injury, and can be quite severe. In these situations, the extent may vary depending on the gaze and head position. In the short term, we often use occlusion—either binasal or spot—to eliminate the double vision and evaluate the visual system weeks later as the visual, and cognitive and control systems come back online. For comitant diplopia, we often investigate the use of prism to attempt to restore single vision. The two cases presented here demonstrate how the use of temporary Frensel prism can get your patients on the road to recovery quickly and effectively.
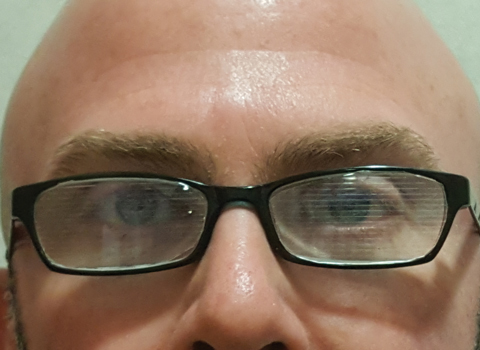 |
| These frames, fit binocularly with Fresnel prism, can be used to restore single vision to patients such as the one in our first case. Click image to enlarge. |
Case One
One morning, a 44-year-old male reported that, several days prior, he was pulling into a parking spot at work, and when backing in, he turned his head to get a better view and suddenly felt different. It turns out, he had a major aneurysm and did something to the blood vessels and supply to his brainstem. Ever since, he had double vision. When he presented, he was wearing an eye patch. Luckily, he was still operating at a high cognitive level, a crucial aspect when considering the use of Fresnel prism.
Visual acuity, confrontation fields, pupils and eye movements were all normal. His primary complaint was the double vision, which he described as “vertical.” Upon visual inspection, the eyes appeared aligned. Cover testing at distance and near revealed a six prism diopter right hypertropia. The magnitude was not changed by altering his head posture or gaze. This was confirmed subjectively and objectively via cover test with loose prism. Not all patients suffering from brain injury double vision can obtain single vision so soon after, so we considered this a good opportunity to use temporary prism. However, the higher the prism strength, the more the visual acuity is degraded. Some patients are not willing or are unable to adjust to the degraded acuity. As his acuity without glasses was excellent, tried frames with plano lenses we had handy.
The use of prism follows a pattern we have presented over and over in this column: less is typically more. Over our careers, we have both found that patients need less prism for fusion than measured on the cover test or even as measured with standard von Graefe or other methods. Giving less prism than measured also serves a therapeutic role in leaving degrees of freedom in which the system can operate.
With two base down over the right eye and two base up over the left eye, the patient reported seeing single vision. We informed him that these were full-time glasses and confirmed with the rehabilitation team that there were no visual restrictions. We checked back several days later and the patient was still smiling. The rehab team reported good progress on balance and hand-eye coordination activities. He will follow up with the vision rehab service at the college in several weeks.
You may be wondering why we chose to split the prism. With a patient who sees well, even though he comprehends the potential for degraded vision, we tend to split the prism to even out the acuity decrease. Essentially, this brings down both eyes equally instead of penalizing one; lessening the visual acuity in one eye would throw off the binocular system we are working so hard to rehabilitate. If one eye has decreased acuity for whatever reason, choosing not to split the prism may be a better option. In that instance, we tend to put the full amount of the prism or the bulk of it in front of the eye with the worse visual acuity or was turned all the time.
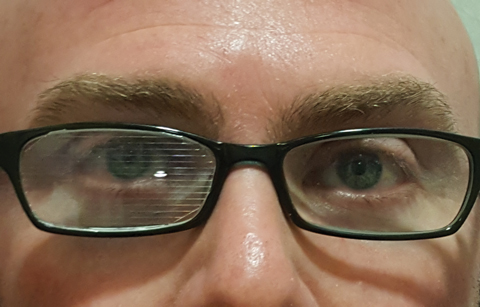 |
| These frames are similar to the ones on page 28, but are only fit monocularly with Fresnel prism. The other lens is plano. Click image to enlarge. |
Case Two
Immediately following the previous patient, a 63-year-old male who suffered a head injury after a fall presented to the clinic. The patient was in good spirits and was joking around with me, which is always a good sign. Unlike the patient described in case one, he was not wearing a patch, indicating that either the magnitude of the diplopia was especially high or fairly low. If the magnitude of the diplopia is large, one of the images may be out of the patient’s line of sight. On the other hand, if the magnitude of the diplopia is small, there is potential that the patient is indeed fusing some of the time. In this case, it was fortunately the latter. As with the first case, the patient was refractively normal. The double vision was intermittent, occurring 50% of the time without a recognizable pattern on the part of the patient or therapists. Cover testing showed a three diopter left hyperphoria.
We grabbed our plano spectacles and Fresnel powers of one and two prism diopters from the kit. Subjectively, the patient reported good fusion with the lower power but felt more comfortable with the higher one. We allowed him to sit with the prism on and questioned him regarding the acuity difference. Since he was thrilled to not see double, he was not fazed by the slight acuity difference. We ended up with two prism diopters base down in the left eye on the plano spectacles and the patient was happy.
The therapists were ecstatic at the improvement in skills several days later. He too will be re-evaluated in several days. We are hoping to either reduce or eliminate the prism if symptoms abated.
Fresnel prisms can aid your patient care regardless of whether or not you treat patients with stroke or traumatic brain injury.
If you are considering grinding in prism, the temporary prism can help confirm the amount needed. In some cases, the use of the prism has a therapeutic effect and the amount of prism can be reduced over time. This is especially true of patients in vision therapy.
For some reason, optometrists seem afraid of prism. With the use of Fresnel prism, this fear should be eliminated.

