 |
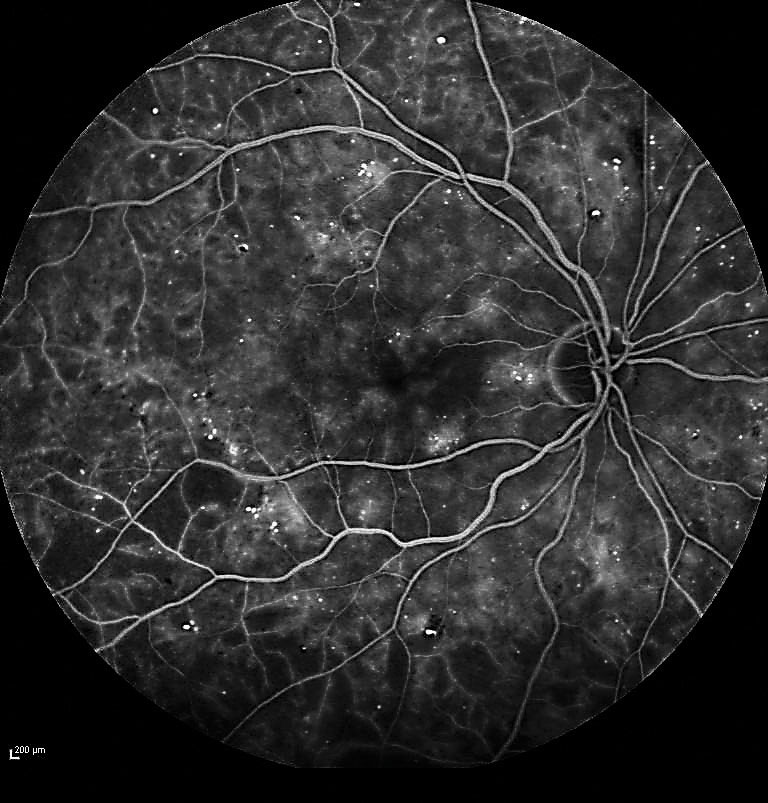
Large areas of capillary non-perfusion may be a sign of more advanced diabetes. Photo: Jay M. Haynie, OD. Click image to enlarge. |
Capillary non-perfusion in diabetic retinopathy (DR) indicates microvascular damage and ischemia, but there is little data on the treatment outcomes with large areas of non-perfusion. In a recent study, researchers aimed to describe the characteristics and treatment outcomes in patients with DR who presented with extensively large areas of capillary non-perfusion.
Fundus fluorescein angiograms (FFA) from 43 eyes of 24 patients diagnosed with DR between January 2017 and December 2019 were reviewed. A large area of capillary non-perfusion was defined as over 70% of capillary non-perfusion throughout the retina.
Seventy-five percent of patients with large areas of capillary non-perfusion exhibited elevated levels of creatinine and urea nitrogen, with 37.5% suffering from hypertension, which indicates that the large areas of capillary non-perfusion may act as a predictive marker for advanced diabetes mellitus with long duration and a lack of proper treatment, the study authors suggested.
“The occurrence rate of large areas of capillary non-perfusion was 3.3%, which accounted for a considerable percentage in the DR population,” they noted. “One possible reason for the high detection rate is that we conducted FFA routinely for the DR population as it provides more information than single fundus photography. It was found that patients with large areas of capillary non-perfusion may present moderate DR on fundus photography showing only microaneurysm, splinter hemorrhage and exudation, which can hardly be distinguished from a mild nonproliferative DR.”
“These patients, if left untreated or improperly managed, may progress rapidly to advanced DR with poor visual function. Our data highlights the necessity and importance of FFA in evaluating the severity of DR, especially in young patients with poorly-controlled diabetes and hypertension, in order to access accurate diagnosis and prompt and effective treatment.”
During the follow-up period, 20 eyes (46.5%) developed severe neovascular complications—vitreous hemorrhage tractional retinal detachment or neovascular glaucoma—and 15 eyes (34.9%) underwent vitrectomy and/or antiglaucoma surgeries. Best-corrected visual acuity of 24 eyes (55.8%) deteriorated, indicating the worsening natural course in eyes, even though ocular and systemic treatment was provided, the authors noted.
“The large areas of capillary non-perfusion may be associated with long duration and poorly-controlled diabetes and hypertension, predict rapid worsening of DR and act as a signal for advanced diabetes with an unfavorable visual prognosis,” the authors concluded. “Early detection and prompt treatments including extensive laser photocoagulation and surgical interventions are recommended, which may potentially slow DR progression and maintain central vision for some time. In addition, we recommend early FFA exam in patients with DR which is necessary for accurate visualization and assessment of retinal microperfusion.”
Huang Z, Qiu K, Yi J, et al. Diabetic retinopathy with extensively large area of capillary non-perfusion: characteristics and treatment outcomes. BMC Ophthalmol. July 4, 2022. [Epub ahead of print]. |

