 |
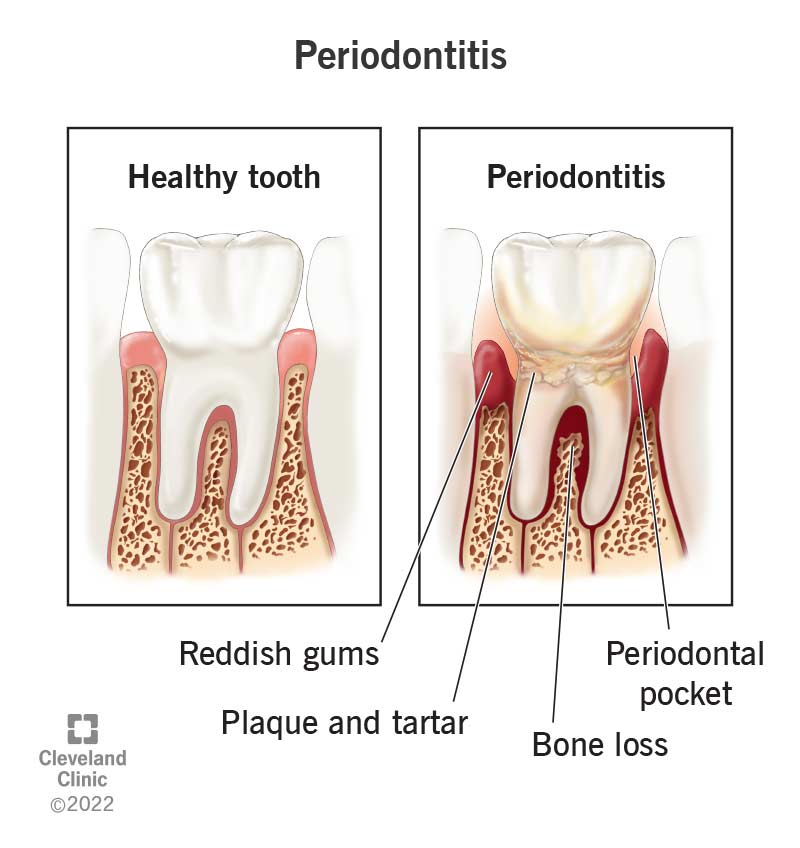
| Bone loss from periodontal disease is the result of an immune response to plaque biofilm and metabolic byproducts. Treatment goals include plaque elimination and reestablishment of a healthy, maintainable oral environment.2 Photo: Cleveland Clinic. Click image to enlarge. |
Gingivitis' more severe counterpart periodontitis has been independently associated with a number of chronic inflammatory markers and causes of systemic inflammation. Researchers recently analyzed its potential association with early biomarkers of degenerative retinal conditions in patients without eye disease. Their findings, published in Ophthalmology Science, suggest that it might be useful to recommend oral hygiene to patients at risk for AMD. 1
The researchers acquired baseline macula OCT images to assess retinal sublayer thickness and used a questionnaire to determine whether patients had very severe periodontitis or not. A total of 4.3% reported very severe gum disease, and these individuals were found to be statistically significantly older and living in areas of greater socioeconomic deprivation, and also more likely to have hypertension or diabetes and currently smoke. Individuals with very severe periodontitis were myopia, on average, while unaffected individuals were hyperopic, on average.
Additionally, the researchers reported that very severe periodontitis was associated with a thinner photoreceptor layer but not in RPE-Bruch’s membrane thickness. The association with a thinner photoreceptor layer was age-modified, where a thinner photoreceptor layer was seen in patients with disease aged 60 to 69, but not among those under 60.
“Our adjusted analysis showed that the photoreceptor layer of individuals with very severe periodontitis was, on average, 0.55µm thinner than that of controls but this was driven predominantly by differences in the 60- to 69-year age group,” the researchers wrote in their Ophthalmology Science paper. “For context, this difference in photoreceptor layer thickness was analogous to approximately five years of age and slightly smaller than the estimate for current smoking (-1.44µm).” They added that photoreceptor layer thinning is a noted feature of late AMD but is increasingly recognized in early disease as well and “may be the earliest manifestation of emerging AMD.”
“Periodontitis is associated with heightened systemic inflammation and addressing it through dental treatments leads to a reduction in inflammatory markers,” they continued. “Given the role of systemic inflammation in the pathophysiology of AMD, it seems plausible that the association between periodontal disease and the outer retinal differences we describe are mediated via this pathway and anti-inflammatory measures may have beneficial effects on outer retinal health.”
They concluded that recommending oral hygiene “may hold additional relevance” for individuals at risk for AMD.
1. Wagner SK, Patel PJ, Huemer J, et al. Periodontitis and outer retinal thickness: a cross-sectional analysis of the UK Biobank cohort. Ophthalmology Science 2024. [Epub ahead of print]. 2. Periodontitis: Key Points. American Dental Association. https://www.ada.org/en/resources/research/science-and-research-institute/oral-health-topics/periodontitis. Accessed January 23, 2024. |

