 |
|
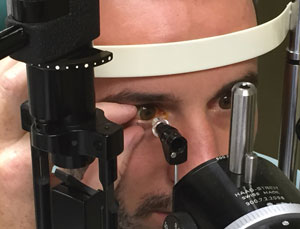
Tonometry readings vary throughout the day and clinicians should consider this inherent instability in their work-ups. Photo: Natalie A. Townsend, OD, and John J. McSoley, OD. Click image to enlarge. |
So much of glaucoma therapy hinges on having an accurate assessment of intraocular pressure (IOP), but clinicians must account for its relationship with central corneal curvature, differing measurement techniques and the influence of corneal biomechanical parameters. Researchers recently reported in Optometry and Vision Science that anterior corneal power change was inversely related to the change in Goldmann-correlated IOP, with myopic and non-myopic eyes reporting a significant but differential IOP impact.
Sixty healthy eyes of 24 patients with emmetropia and 36 with myopia were recruited for this cross-sectional study. Both anterior and posterior central corneal powers of the steep (Ks), flat (Kf), mean meridian, best-fit sphere and central corneal thickness were recorded, followed by IOP (Goldmann-correlated and corneal-compensated) and corneal biomechanics (corneal hysteresis and corneal resistance factor). Measurements were obtained every three hours between 9:30AM and 6:30PM.
Group mean, amplitude of change and the diurnal change in Goldmann-correlated IOP were 15.14mm Hg, 3.33mm Hg and 1.81mm Hg, respectively. Overall, an IOP increase was associated with a decrease in the adjusted anterior corneal power. Myopic eyes were associated with a decrease of 0.04D in Ks and 0.03D in Kf per 1mm Hg increase in IOP, whereas a 1mm Hg increase in IOP for those with emmetropia only flattened the Kf by 0.03D.
“Findings from this study indicate that it is worthwhile to observe the association between diurnal change in IOP and corneal power,” the study authors wrote in their paper. “Clinicians must keep in mind the impact of large IOP fluctuation on the anterior corneal power.” Even a 1.6 mm Hg mean IOP fluctuation is related to faster visual field progression in myopic normal tension glaucoma eyes compared to non-myopic ones, they point out. Likewise, 1mm Hg higher IOP fluctuation has been shown to be associated with a 31% higher risk of glaucomatous visual field loss progression.
“To date, this is the first report demonstrating the inverse association between increasing intraocular pressure and corneal curvature after adjusting for corneal biomechanical properties and thickness in a clinical setting,” the researchers pointed out.
Biswas S, Biswas P. Relationship between diurnal variation in intraocular pressure and central corneal power. Optom Vis Sci. December 14, 2022. [Epub ahead of print]. |

