 |
Q: I have a patient who had a successful graft nearly 20 years ago and now appears to have keratoconus in the graft again. The graft is thin, small and very steep. What factors pose a risk for recurrence?
Anat Galor, MD, MSPH, of the Bascom Palmer Eye Institute, recently saw a similar case that she hopes will help steer other optometrists in the right direction when caring for these types of patients.
Case Details
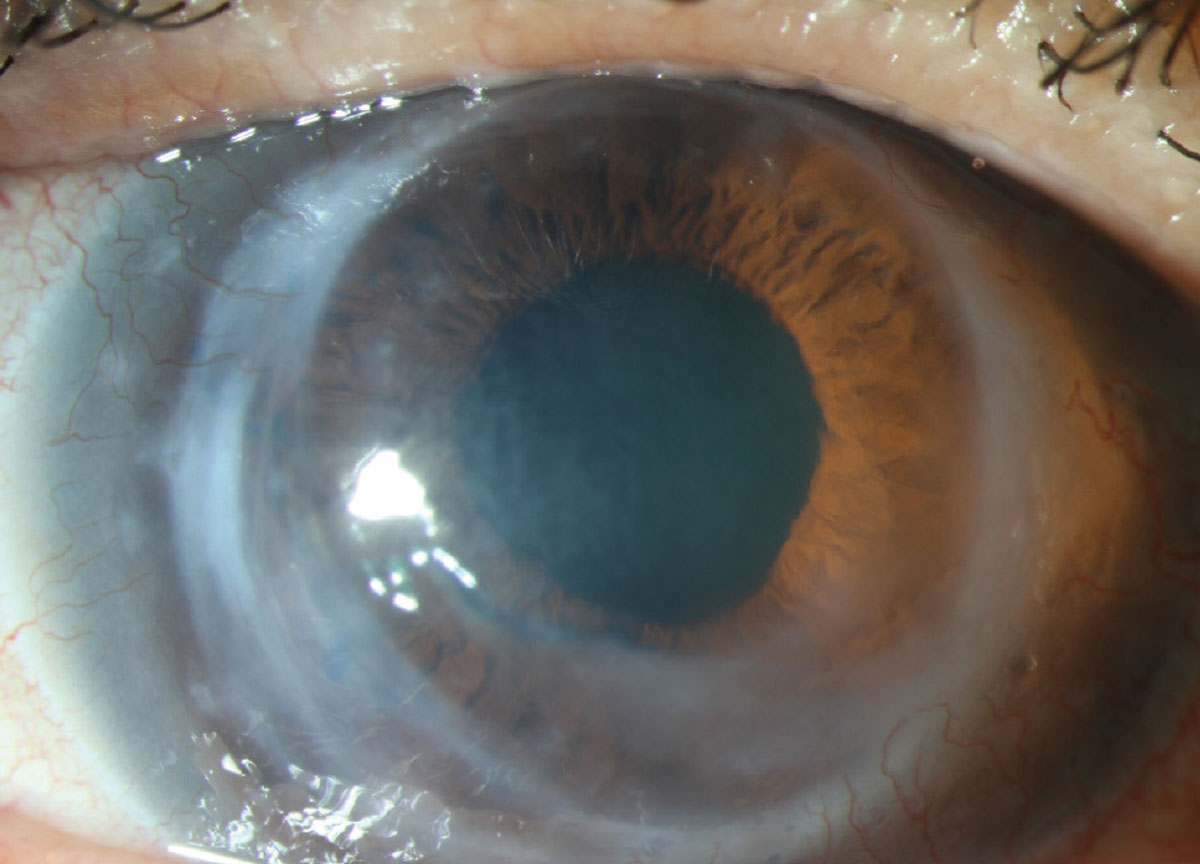 |
| Fig. 1. Corneal ectasia in a graft performed 36 years prior for keratoconus. Click image to enlarge. |
A 70-year-old white male presented to the clinic with decreased vision that began while being fit for a hard contact lens in the right eye. His past medical history was significant for keratoconus in both eyes, and he had undergone a corneal transplant in 1983 in the right eye.
On presentation 36 years after the original transplant, best-corrected visual acuity with contact lenses was 20/30 in the right eye and 20/20 in the left eye.
Over the next few months, increased corneal haze and progressive ectasia were noted in areas of the inferior temporal graft-host junction, and a decision was made to proceed with repeat penetrating keratoplasty, cataract extraction and intraocular implantation (Figure 1).
During the surgery, the area of ectasia was removed using an 8.00mm trephine and an 8.25mm donor cornea was sewn into place (Figure 2). In 2021, two years after surgery, the patient’s best-corrected visual acuity was 20/20 with a contact lens. No recurrent ectasia was noted. However, in looking back at the case, what are the risk factors leading up to the occurrence of recurrent ectasia in a graft?
Risk Factors
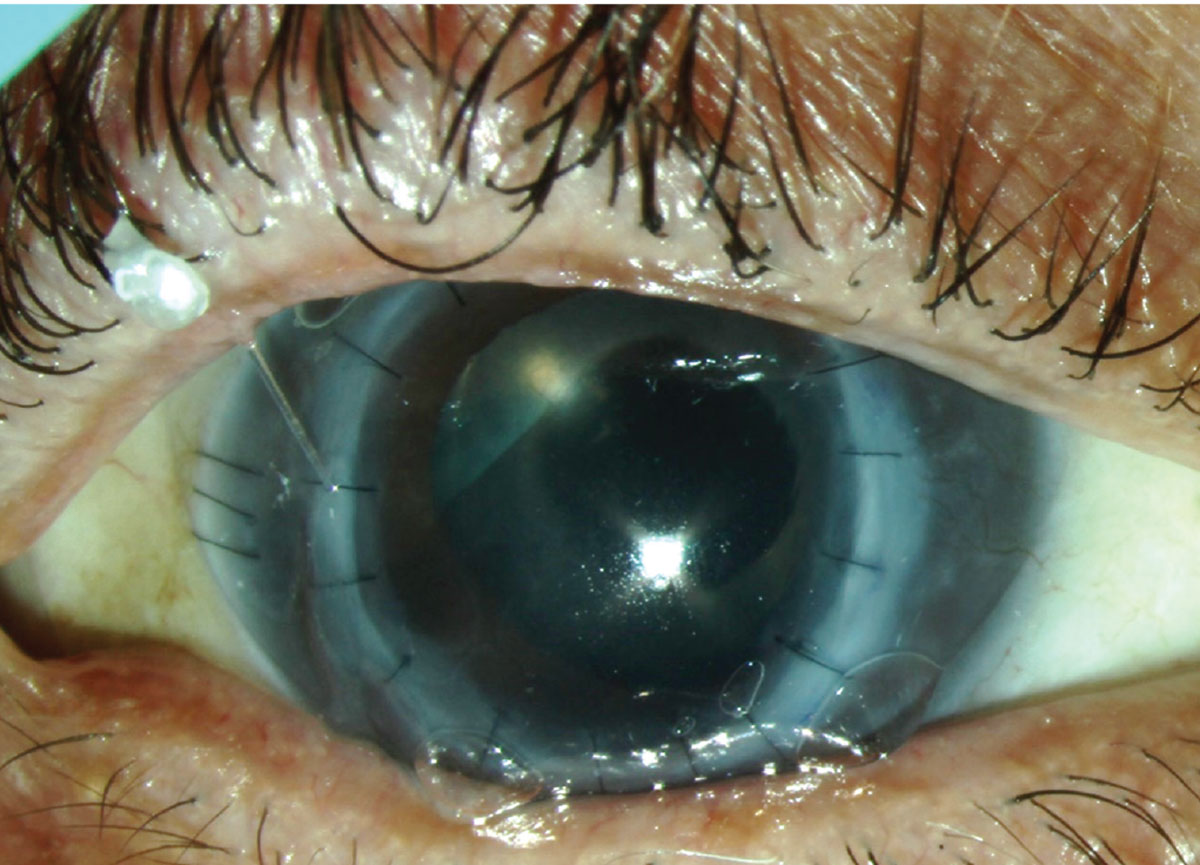 |
| Fig. 2. Repeat corneal transplantation and cataract extraction performed with area of ectasia removed. Click image to enlarge. |
The short answer is that risk factors for recurrent ectasia after penetrating keratoplasty are unknown, says Dr. Galor. However, she notes that this finding typically occurs along the inferior graft-host junction, suggesting that progressive ectasia occurs within the residual host tissue. This may explain why ectasia is more commonly described in cases of small grafts, as more host tissue remains in the periphery, she adds.
If caught early, riboflavin-assisted crosslinking can be considered in the area of ectasia, with care to avoid the limbus, according to Dr. Galor. However, when significant as in this case, she suggests repeat corneal transplantation can be performed, making an effort to include as much of the ectatic area as is feasible in the trephination.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
