 |
In this current issue, one of us (SB) coauthored a CE article entitled “When It’s Not Amblyopia: The Differential of Functional vs. Pathological Vision Loss.” This, as well as many of our prior columns, highlight some of the significant issues that arise when pathological vision loss is missed because functional vision loss (amblyopia) is the suspected diagnosis. It seems, unfortunately, to be a recurrent problem in eyecare. In this month’s case, the misdiagnosis of amblyopia in a young girl sadly resulted in blindness in one eye and significant field loss in the other eye.
Case
An 11-year-old girl presented for an eye examination because the mother reported that her eyes were not straight. She had been noticing this for a while and was becoming concerned.
Entering uncorrected visual acuities were 20/100 in OD and 20/20 OS. Cover test revealed a right exotropia at distance and at near. The refractive error was OD: -0.75-0.75 x 90, with best-corrected visual acuity (BCVA) of 20/70 and OS: -0.50 sphere, with BCVA of 20/20. The eye doctor in this case used a “check-off” type of recording form in which the results were not written out but checked off, indicating (according to the doctor in his deposition) that the test was performed and the results were normal. At this visit, everything was “checked,” including the disc, macula and tonometry.
 |
|
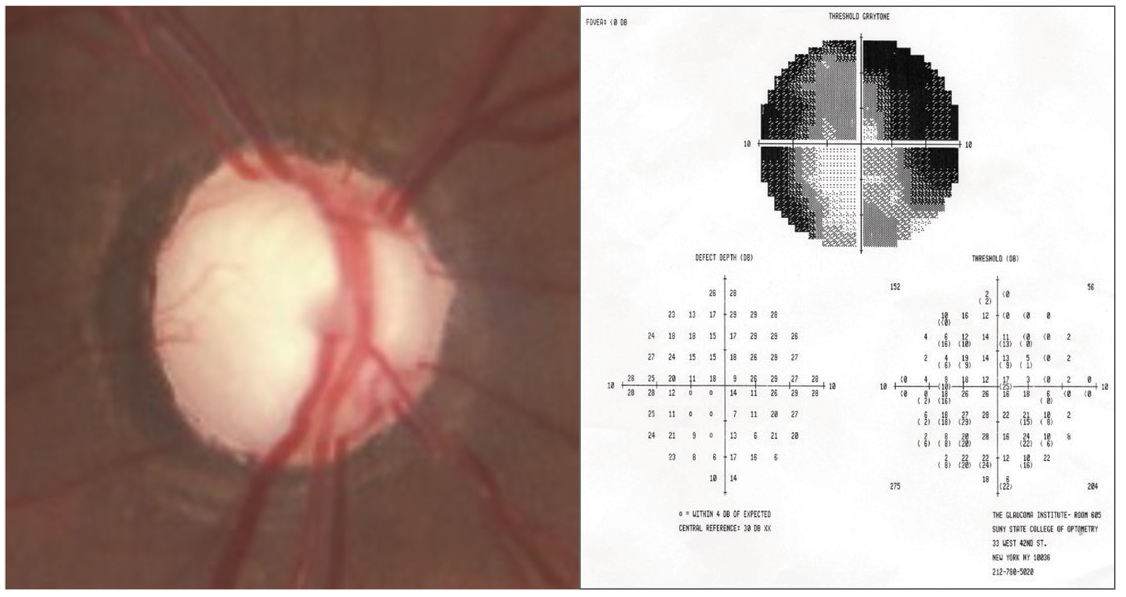
Fig. 1. Cupped out disc in end-stage glaucoma, with corresponding 10º visual field in another patient. Click image to enlarge. |
Phorias at distance and near were attempted but not measured due to suppression of the right eye in the phoropter. A Keystone Visual Skills test was also performed, and the doctor noted “ Dog over Pig”for Card #1, in which one eye sees the dog and the other eye sees the pig and “three ball fusion response at distance and near.” On the phoria cards at distance, the doctor noted that the arrow pointed to #15 (one eye sees the arrow and the other eye sees numbers), indicating a high exophoria or an underconvergence response, and at near, the arrow pointed to between #6 and #7, indicating an ortho to slight exophoria response.
The diagnosis was not indicated, but the eye doctor wrote in the chart, “VT (vision training) suggested—no decision.” Apparently, the doctor thought the patient had a functional reason for the vision loss, namely exotropia, and suggested vision training.
The patient never returned for VT (it was later learned that the parents thought the fee for VT was too expensive) and presented for another eye examination over two years later. Her chief complaint at this visit was that when she covers the left eye, the right eye is blurry. BCVAs were 20/400 OD and 20/20 OS. At this visit, instead of using a check-off form, ophthalmoscopy results were written and were recorded as “OD extreme cupping” and “OS moderate cupping.” Tonometry readings, performed by non-contact tonometry, were 51mm Hg OD and 49mm Hg OS. The patient was immediately referred to an ophthalmologist, diagnosed with end-stage juvenile open-angle glaucoma (JOAG) OD and advanced JOAG OS. Despite medical and surgical intervention, the glaucoma progressed, resulting in hand-motion vision in the right eye with no remaining visual field and 20/20 in the left eye with a 30% reduction in the visual field.
Malpractice Allegation and Outcome
The eye doctor was sued for failure to detect the glaucoma two years earlier. The case was settled for $350,000 two days before a jury trial.
You Be the Judge
Considering the facts presented thus far, opine the following questions:
Did the eye doctor have a reason to diagnose amblyopia, since the patient had a right exotropia and not an exophoria on cover test?
Did the results on the Keystone Visual Skills test support a diagnosis of amblyopia?
Should the eye doctor have recorded quantitative data for IOP measurement and optic nerve head findings, or is a checkmark enough when findings are normal?
Are the patient and her parents responsible for not returning for the recommended vision training, which would have given the doctor another opportunity to reassess the situation?
Is the eye doctor culpable for malpractice, since he failed to diagnose glaucoma in a young child, which is a very rare condition?
Is tonometry the standard of care prior to the teenage years?
What would a like practitioner under like circumstances have done on the first visit?
Our Opinion
JOAG is rare, with a reported prevalence of one in 50,000 in the US. 1 It occurs in individuals younger than 40 years of age.2 Therefore, when a young child presents with reduced vision in one eye, end-stage JOAG is not foremost as the likely explanation for reduced visual acuity. However, before amblyopia can be diagnosed, certain criteria apply.
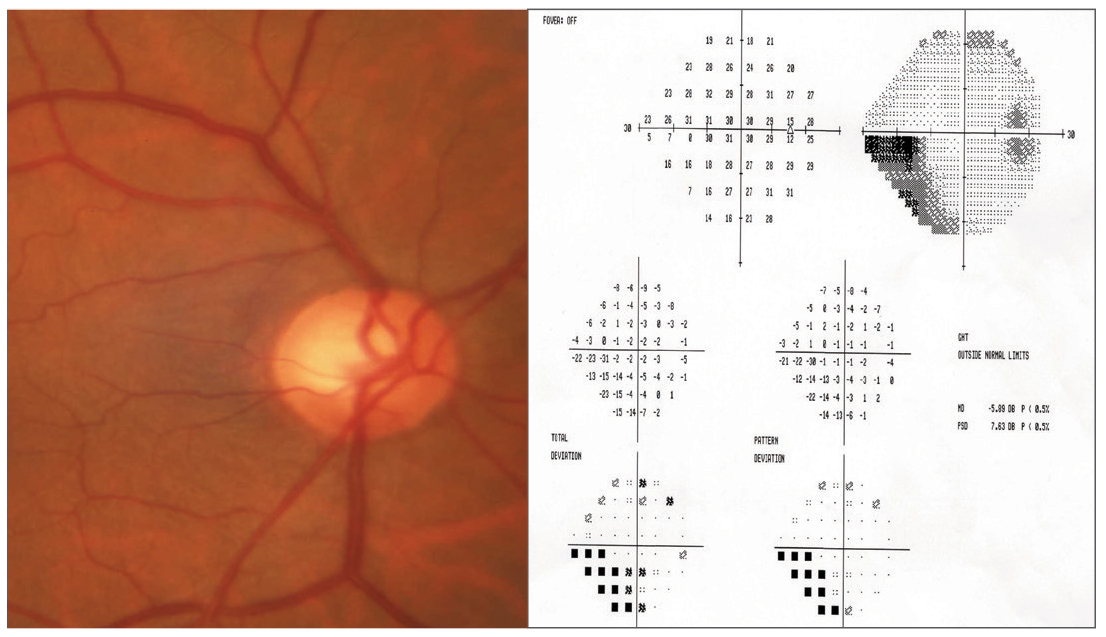 |
| Fig. 2. Cupping in moderate glaucoma in with corresponding 24-2 visual field in another patient. Click image to enlarge. |
One of us (JS) reluctantly opined that the eye doctor had no explanation for the reduced visual acuity in the right eye. “Reluctantly” because this case dates back four decades, and it was unclear what a “like practitioner” would have concluded under like circumstances. The standard of care continues to evolve, and today this would clearly be a violation of the existing standard of care.
While strabismus existed, most patients with exotropia can and do alternate, unless the turn is so large that the exotropic eye is completely suppressed. The eye doctor noted on Keystone Skills that there was no suppression, since the child saw both the dog and the pig, as well as the arrow and numbers on the phoria card. Therefore, the turn was not large enough for suppression, and the exotropia was very unlikely the reason for the reduced visual acuity in the right eye. There was only a slight difference in refractive error between the two eyes, and therefore, refractive amblyopia was not the reason for the reduced visual acuity. The eye doctor failed to record the pressures in the eye on the first visit, noting tonometry as “checked” and neither did he record any details about the discs and maculas at this initial examination.
Discussion
The eye doctor is culpable on a few issues:
First, he had no good explanation for the reduced visual acuity in the right eye. There was no significant anisometropia, and the strabismus was an exotropia, not an esotropia. If the child was able to perceive two targets on the Keystone Skills battery, then she was not suppressing. And most exotropes can and do alternate. This is important to remember when attributing decreased visual acuity to exotropia.
Second, the eye doctor did not record the appearance of the optic nerve heads in his initial examination or his tonometry findings but instead checked it off in his record. These “checks” were of no help in his defense since they did not indicate a quantitative amount that could have been compared from one examination to the next.
Third, he did not specify a diagnosis in his initial examination, and he did not specify a recall date except to write “VT suggested—no decision.” Children with reduced vision in one eye should be monitored closely if they are not referred and if the cause is not evident.
Since there was no other reason for the reduced acuity in the right eye, it is likely the child already had end-stage glaucoma in her right eye at the initial examination as the visual acuity was already affected. Likely, the disc was already cupped out, since the VA was reduced (Figure 1). Since the visual field in the left eye was reduced by 30%, she likely had moderate glaucoma in the left eye two years later (Figure 2). But more important, the delay of two more years resulted in a further decrease of central vision in the right eye and additional loss of visual field in the left eye-her only good seeing eye.
This case dates back decades, but knowledge of such cases will likely prevent similar cases in the future.
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.
1. Roth AM. Histoplasma capsulation in the presumed ocular histoplasmosis syndrome. Am J Ophthalmol. 1977;83(3):293-8. 2. Macular Photocoagulation Study Group. Argon laser photocoagulation for ocular histoplasmosis. Arch Ophthalmol. 1983;101(7):1347-57. 3. Gabel W. Vicarious liability. J Am Optom Assoc. 1987;58(7):599-601. |

