 |
Betsy is a 50-something woman with cerebral palsy, including a degree of cognitive impairment, who lives with her devoted sister who serves as a caretaker. A two-decade-old eye exam in a different state revealed VA of no light perception (NLP) OD and 20/50 OS and myopic degeneration. Later, when her sister was asked about Betsy’s previous vision, she commented that Betsy knew her colors, was able to make sandwiches, walk down to the mailbox, pick up the mail and was able to recognize family names on envelopes and to distribute without error the letters to her sister or her sister’s husband. Betsy was very proud of herself to be able to perform this task. According to her sister, Betsy was also able to “walk freely around Walmart.”
Case
Betsy’s first recent exam with the family’s local eye doctor revealed VA of NLP OD and counting fingers vision OS, but the doctor noted accurate VA measurements were difficult. Betsy’s sister reported to the doctor that she was able to sit in front of a TV, “watch” and enjoy several shows. The sister also mentioned that Betsy does not like to be examined and is generally uncooperative. The record included the notation, “Extremely shallow anterior chamber,” no visible pupil in the OD but only iris. A nondilated retinal exam revealed 0.3 cup-to-disc ratio OS and no other notations. IOP was recorded at 17mm Hg OS. Glasses were prescribed with a balance lens in the OD and -16.50D=-2.00D Cx 180 OS. The next exam took place three years later and it yielded very similar results including the statement, “Extremely shallow anterior chamber.”
About a year later, during the holiday season, Betsy communicated to her sister that her eye was hurting a lot. Several hours later, she was evaluated by a physician’s assistant (PA) in the emergency department (ED) of a nearby hospital. The PA recorded that she observed that the left eye was “red” and had a “small corneal abrasion.” Azithromycin eyedrops were recommended as was a follow-up with her eye doctor within 48 hours. The supervising MD in the ED never directly evaluated Betsy, knew that eye pressures were not obtained and noted that they “reviewed the documentation, treatment plan and medical decision making” of the PA and agreed with it.
 |
|
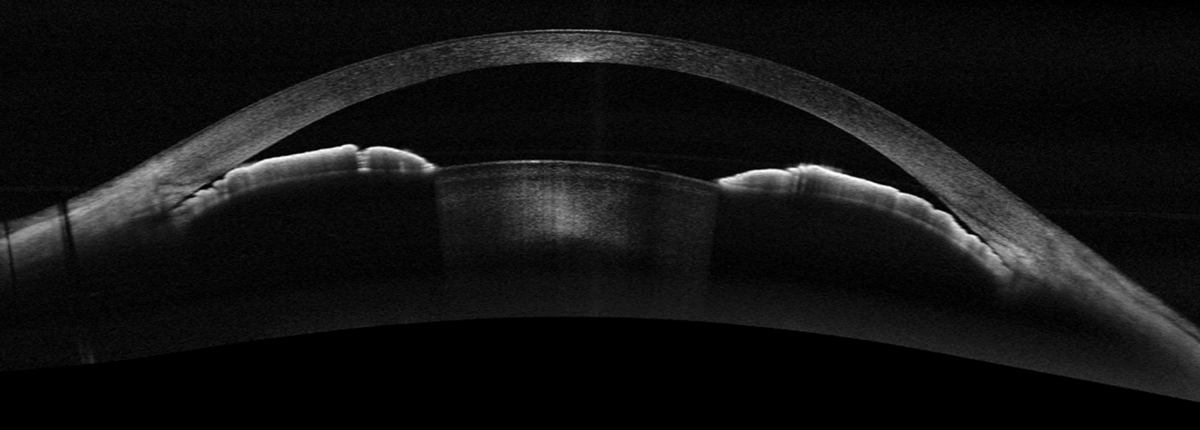
Widefield OCT in a different patient with a narrow angle with iridotrabecular contact. Photo: Michael Cymbor, OD, and Emilie Seitz, OD. Click image to enlarge. |
The next day, the family eye doctor examined Betsy and recorded the chief complaint as “pain right now” but could not identify a corneal abrasion. He then gives the sister the name of a cornea specialist written on a prescription pad and said, “If the pain gets worse, call the cornea specialist.” He told the sister caretaker to continue with the azithromycin eye drops. The sister later testified that the exam took about 20 minutes and that the doc did a lot of “prodding” but the record only reveals “pain right now…? corneal abrasion.”
The sister slept with Betsy half that night and Betsy continued to complain of lots of pain. Betsy woke up on the morning of January 1 and according to the sister, she was now blind. She got out of bed to go to the bathroom but couldn’t find it and yelled, “I can’t see!” Panicked, the sister rushed Betsy to the same ED. A different emergency physician noted Betsy’s left pupil to be dilated and nonreactive with “minimal light-dark discrimination.” On this visit, IOP was 38mm Hg OS. This clinician concluded that Betsy most likely had acute angle-closure glaucoma OS and immediately arranged for transportation via helicopter to a major medical center with ophthalmic surgeons readily available even though it was the early morning of New Year’s Day.
Soon after, a glaucoma specialist diagnosed intermittent angle-closure glaucoma OS. Treatment with Diamox (acetazolamide, Duramed Pharmaceuticals) and several topical meds were successful in lowering the IOPs to below 10mm Hg. Visual acuity over the next several months was light perception at best. Ophthalmic ultrasound about a year later revealed chronic retinal detachment with vitreous membranes OD and phthisis bulbi OS following a chronic retinal detachment.
You Be the Judge
Based upon the information available thus far, what is your opinion?
- Should have the family eye doc referred based upon the “extremely narrow anterior chamber” in the left eye of this monocular patient that was noted on two occasions?
- Should a dilated fundus examination (DFE) be performed on a 16D myopic patient such as Betsy, even though she was quite difficult to examine?
- Are ED personnel trained to perform IOP measurements?
- Can the hospital and its personnel as well as the family eye doctor all be found culpable of malpractice in this case?
Our Opinion
Although angle-closure glaucoma is far more common in high hyperopes than in very high myopes, it does occasionally occur and an “extremely narrow anterior chamber” such as documented in this case, cannot be ignored. A laser peripheral iridotomy (LPI) should have been considered years earlier. If an LPI was performed following the first visit four years prior it is more likely than not that the chronic angle-closure glaucoma could have been treated successfully and the patient would still have useful vision as documented by her sister prior to this unfortunate incident.
One could argue that monocular patients deserve an even more careful assessment. Determining why a patient has a blind eye is always highly recommended and may prevent a similar outcome in the seeing eye. Although more difficult in some mentally and physically challenged patients, comprehensive exams should be performed or at least attempted. Patients with narrow angles should have gonioscopy performed or at least tried, patients with very high myopia deserve a DFE with binocular indirect ophthalmoscopy. When appropriate, such as in this case, referral to a more highly trained, experienced and skilled clinician should be considered.
 |
|
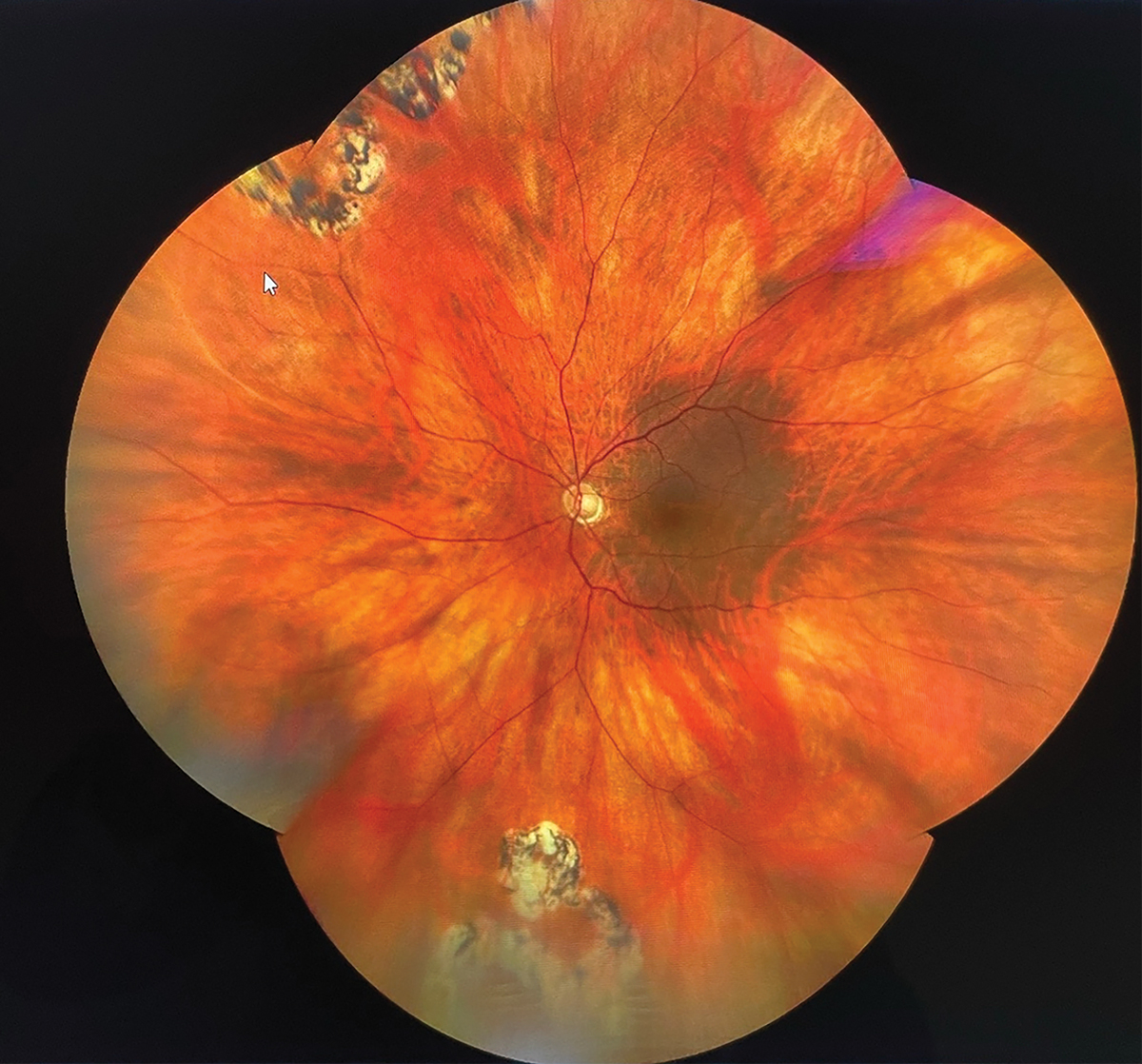
Fundus image of a pathological myopic eye with two superior tears and two inferior tears treated with laser successfully. Click image to enlarge. |
One of us (JS) was requested to review all the information available in this case and concluded that the hospital and several of its personnel (the PA and the supervising MD on the first visit) failed the patient. Opinions regarding the standard of care in the ED would need to be made by ED personnel with similar backgrounds. When asked about measuring IOPs in the ED, the PA testified that she learned how to measure IOPs but rarely if ever performed this procedure in the ED, because she did not feel comfortable undertaking it, especially in a difficult patient. She also mentioned that tonometry should not be performed in a patient with a corneal abrasion. The supervising MD did not believe IOP measurements were necessary, since the PA observed a corneal abrasion and concluded that the symptom of pain was secondary to the corneal abrasion. The MD believed it was appropriate to refer the patient back to their family eye doctor within 48 hours for follow-up.
It is our opinion that there is no viable defense for the family eye doc to examine this patient still complaining of pain, referred by the ED with a diagnosis of a corneal abrasion, not able to find a corneal abrasion even with a slit lamp biomicroscopy with fluorescein dye and not go to the next logical step and perform IOP measurements. Suggesting a follow-up with a cornea specialist if the pain persists is somewhat unrealistic on New Year’s Eve.
Outcome
In cases such as this, with an outcome of blindness, the defense attorneys make every effort to identify well-regarded experts who could somehow defend the hospital and doctors involved. One expert concluded that the cause of blindness was the retinal detachment and not the glaucoma. However, a review of the timeline clearly documents that the retinal detachment and phthisis bulbi occurred many months after the IOPs of 38mm Hg and the diagnosis and treatment of the chronic angle closure glaucoma. Another expert for the hospital argued that the pain on the first ED visit was due to a corneal abrasion that was treated appropriately and successfully and that the pain reported to the family eye doc the next day—the one who could not find the abrasion—was due to angle-closure glaucoma. Furthermore, it was argued, the diagnosis and treatment were entirely appropriate on the second visit to ED.
The case was settled prior to jury trial for several million dollars, split between the insurance companies for the hospital and the family eye doc. A blind patient at trial typically invokes sympathy, resulting in large jury awards.
And, yes, an extremely narrow anterior chamber is a disaster waiting to happen.
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.

