 |
|
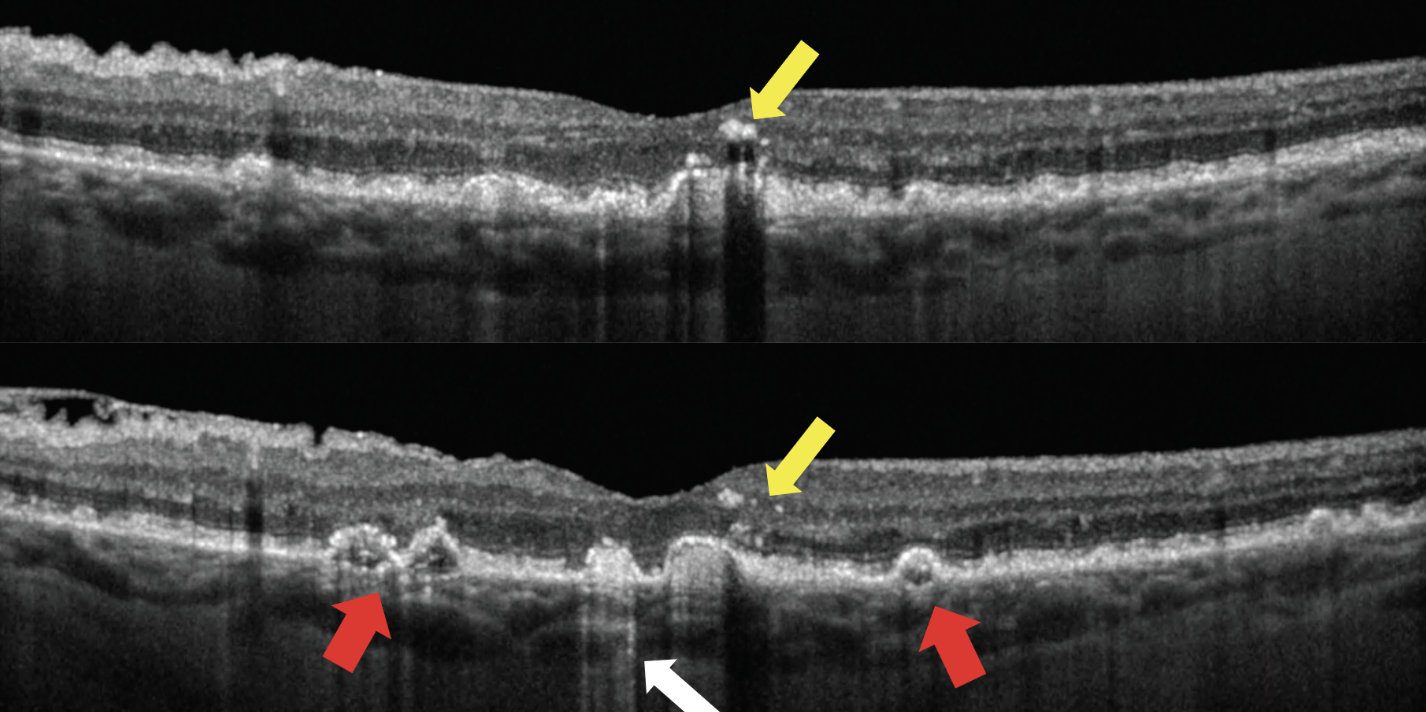
Given that intraretinal hyperreflective foci are a sign of distressed RPE, the researchers weren’t particularly surprised that complete retinal pigment epithelium and outer retinal atrophy frequently ensues in this location. Photo: Jessica Haynes, OD. Click image to enlarge. |
There has been significant interest in developing treatments targeting earlier stages of geographic atrophy (GA). There has also been an intense focus on biomarkers identified on OCT that may increase the risk for development of GA, such as intraretinal hyperreflective foci, high central drusen volume, soft drusen/drusenoid pigment epithelial detachments (PEDs), acquired vitelliform lesions, hyporeflective core drusen, thin double-layer sign due to thickened basal laminar deposit and subretinal drusenoid deposits. Researchers based out of the Doheny Eye Institute in Pasadena, CA performed a lesion-level analysis to define which OCT biomarkers were associated with increased risk for the development of complete retinal pigment epithelium and outer retinal atrophy at that location using a case-control approach within the same eye. They determined that, in patients’ eyes with early or intermediate AMD, the presence of intraretinal hyperreflective foci, drusenoid PED, and a thin double-layer sign appears to increase the risk of development of complete retinal pigment epithelium and outer retinal atrophy at that location over four years.
The study included a total of 57 eyes of 41 patients with dry AMD and evidence of complete retinal pigment epithelium and outer retinal atrophy were included. Mean time from the baseline visit to the first visit with complete retinal pigment epithelium and outer retinal atrophy was 44.7 months.
The presence of soft drusen, drusenoid PED, acquired vitelliform lesions, thin double-layer signs and intraretinal hyperreflective foci at the baseline visit was all associated with a significantly increased risk of complete retinal pigment epithelium and outer retinal atrophy at that location. Multivariable logistic regression revealed that intraretinal hyperreflective foci (odds ratio; OR: 8.56), drusenoid PED (OR: 7.15) and a thin double-layer sign (OR: 3.48) were independent predictors of development of complete retinal pigment epithelium and outer retinal atrophy at that location.
“It is notable that intraretinal hyperreflective foci appeared to be a substantially stronger risk factor for local progression to atrophy compared with drusenoid PED,” the study authors wrote in their paper. “This might suggest that these were a later phenotype/precursor or feature that appears more proximal to the time of development of atrophy compared with drusenoid PED.”
“As these lesions appear to be important precursors for the development of atrophy, they may be useful for informing a more granular OCT-based staging system and for defining new endpoints for potential future early therapeutic intervention,” the researchers concluded. “It could also provide new insights into the pathophysiologic mechanisms and sequence of events leading to the development of GA.”
Manafi N, Mahmoudi A, Emamverdi M, et al. Topographic analysis of local OCT biomarkers which predict progression to atrophy in age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. February 1, 2024. [Epub ahead of print]. |

