A large number of ophthalmic conditions can be treated with topical and oral pharmaceutical agents. But we need to keep in mind that when we discuss “topical” and “oral,” we are not so much discussing medications directly but rather we are describing routes by which medication can be delivered. In fact, several medications, such as steroids for example, can be delivered in a variety of ways. We are familiar with topical and oral steroid uses, but many of those same steroids can be delivered by way of injection, inhalation and transdermal administration.
This article focuses on our third most common route of administration of medications used to treat conditions of the eye and adnexa: injections.
Reasons for Injections
Diagnostic Injections
Primary Therapeutic Injections
Secondary and Adjunctive Injections
Just as in the use of oral and topical medications, injectable medications can be divided into those that are used for diagnostic purposes and those that are used for therapeutic purposes. And, of those injectable medications used for therapeutic purposes, they can be further divided into primary treatment therapies and adjunctive treatment therapies. (See “Uses of Eye Care Injections.”)
Uses of Eye Care Injections
• IV fluorescein angiography
• IV indocyanine green angiography
• IV Tensilon testing for myasthenia gravis
• Intradermal TB testing
• IM antibiotics for gonorrhea
• Translesional steroids for chalazia
• Subcutaneous anesthetics for the periocular region
• IM/subcutaneous botulinum toxin
• Intravitreal injections for AMD
• Intravitreal injections for macular edema
• SC, IM or IV epinephrine for anaphylaxis
• Subconjunctival steroids for uveitis
• Sub-Tenon’s injections of steroids for uveitis, pars planitis, posterior pole inflammations
• Intravitreal injections for AMD and macular edema
When using oral and topical medications, the onus of proper medication administration usually falls on the shoulders of the patients, and we as eye care providers often give too little thought to the actual delivery of the treatment. However, when utilizing injectable medications for managing eye conditions, the onus of proper administration of the injectable medications falls squarely on the shoulders of the provider. As such, any eye care provider who utilizes injectable medications must be trained in the proper administrative techniques involved.
In addition, the provider obviously must be familiar with the medications themselves—including dosages, indications, contraindications, side effects and expected outcomes—as well as manage complications that result from their administration.
So, it is absolutely imperative that eye care providers who utilize injections are trained in the actual techniques of injectable administration because there are many types of injections germane to eye care. Furthermore, state licensing laws must be adhered to when prescribing any medications. (See “Authority of Optometrists to Administer Drugs Via Injection,” below)
Types of Injections
The types of injections used for conditions of the eye and adnexa include intramuscular, intradermal, subcutaneous, subconjunctival and sub-Tenon’s, intravitreal, intravenous and intracameral injections.
Let’s look at each in turn.
Intramuscular Injections
When we think of intramuscular (IM) injections, we tend to think of significant volumes of medication delivered through large, long needles into the muscles of the extremities. But this type of IM injection has relatively limited use in eye care.
Often, IM injections in the setting of eye care are used to treat systemic infections that have ocular manifestations, such as gonococcal infections, in which the typical treatment consists of an IM injection of Rocephin (ceftriaxone, Roche).1-3 Locations for placement of these IM injections are the deltoids and quadriceps femoris muscles, and the hip.3
Sometimes, IM injections are used to treat contact dermatitis reactions of the eye and adnexa, as in cases of poison ivy, for example.
Nowadays, one of the more common types of facial injections is also technically an intramuscular injection. These injections are most often utilized by dermatologists and plastic surgeons for cosmetic purposes.4-6 Botox Cosmetic (onabotulinumtoxin A, Allergan) for the reduction of glabellar lines and facial wrinkles falls into this category. Botulinum toxin interrupts the normal neuromuscular junction transmission, resulting in paralysis of the striated muscle supplied by that neuromuscular junction (NMJ).

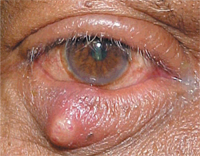
Botox is used not only for cosmetic purposes but also for therapeutic purposes, such as hemifacial spasm (pictured here), blepharospasm and migraine headaches.
Ideally, Botox is administered directly into the desired muscle, making it an IM injection. However, Botox is often administered as a subcutaneous facial injection in the tissue overlying the target muscle, and diffusion of the neurotoxin into the underlying muscle produces the desired effect.
While Botox is often considered a cosmetic treatment, there are indications where Botox is used for therapeutic purposes, such as blepharospasm, hemifacial spasms, extraocular muscle disturbances and, most recently, migraine headaches.5,7 While the actual mechanism of headache reduction is unknown, botulinum toxin is believed to block nocioceptive neuropeptides, which are released in situations of chronic type pain.
Intradermal Injections
This type of injection has limited use in eye care. Because intradermal tissue is poorly vascularized, it is a good site for observing localized immune-type reactions, such as those that occur when purified protein derivative (PPD) testing is used to determine an individual’s exposure to tuberculin.

A general example of intradermal injection: Placement of this injection involves inserting the needle bevel slowly at a 5° to 15° angle. The needle bevel is advanced through the epidermis, just under the skin surface, so that the entire bevel is covered. Photo: CDC/Gabrielle Benenson
Subcutaneous Injections
The subcutaneous tissue lies beneath the dermis and above the muscle tissue. It consists of connective tissue and fat, and is minimally vascularized. It is not tightly adherent to the over- and underlying tissues and, as such, can hold larger volumes of medications.
Injectable anesthetics are administered subcutaneously in the periocular tissues. These may be delivered as a local type of injection (targeting a specific area, such as the temporal aspect of a lid), or as a more regional, nerve block injection, targeting a larger area. These are used primarily for anesthesia of the upper and/or lower eyelids during repair of lacerations, biopsy of lesions, removal of foreign bodies of the lid, electroepilation, chalazia removal and thermal punctal cautery.
The subcutaneous tissue of the eyelid, because of its physical characteristics (ability to hold larger volumes of medications) and its close proximity to the tarsal plate, make it an ideal tissue reservoir for steroids to treat chalazia. Chalazia are inflammatory processes of the meibomian glands.
They may begin spontaneously due to localized irritation, but most often develop following an infectious process.
Steroids are useful in the management of chalazia, but they are contraindicated in active infectious eyelid processes. Therefore, when considering an injectable steroid for the treatment of an eyelid “stye,” make sure that the condition is in fact a chalazion and not something else.


Subcutaneous injections are used to anesthetize the eyelids for repair of lacerations, biopsy of lesions, removal of foreign bodies of the lid, electroepilation, chalazia removal and thermal punctal cautery.
From an anatomical perspective, chalazia develop within the meibomian gland. Meibomian glands are located within the tarsal plate. The tarsal plate consists of loose connective tissue, and is cartilaginous in nature.
As such, it is rather dense, and inserting a fine needle into tissue of this density is difficult. However, as chalazia develop, they invariably enlarge in the x-, y- and z-axes.
Some chalazia may “point” internally more than externally, and some vice versa.8 With either presentation, the most appropriate location for the administration of the injectable steroid is still the subcutaneous space.
On the conjunctival side of the lid, the tarsal conjunctiva is tightly adherent to the underlying tarsal plate, and as such, there is very little subconjunctival space. Attempting to administer an injectable steroid into this space is difficult at best.
While chalazia vary in size, duration and firmness, steroid injections generally work very well if two conditions are met: the appropriate amount and concentration of steroid is used, and the chalazion is of recent origin (generally less than four to six months) and so is still relatively soft. As a chalazion becomes more compact over time and more granulation tissue develops inside the affected meibomian gland, it becomes more dense. These respond more slowly to steroid injections, and may require a second injection. Older chalazia––especially if they have been present for longer than six months––may not respond to steroids and must be incised and drained or excised.
A chalazion may “point” externally more than internally (or vice versa). Regardless, the steroid is injected into the subcutaneous space. Photo: Thomas J. Stokkermans, O.D., Ph.D.
The most effective steroid for the treatment of chalazia is Kenalog-40 (Bristol-Myers Squibb), which is triamcinolone acetonide in a 40mg/cc concentration. Kenalog-40 is a thick, viscous, white suspension, and is not quickly absorbed into the systemic circulation. It is ideal for the treatment of chalazia for this and several other reasons. While the eyelid subcutaneous space can hold a (relatively) larger volume of injectable medications, what is administered in this area should be not excessively voluminous. Depending on the size and duration of the chalazion, anywhere between 0.2cc to 1.0cc of Kenalog-40 is used.
Because it is a viscous suspension that is slowly absorbed, the bolus of medication tends to sit in the subcutaneous space for an extended period of time, and gradually works to reduce the chronic inflammatory response that is the basis of the chalazion’s recalcitrance. As such, it is quite normal to be able to visualize the triamcinolone remaining under the dermis and epidermis of the lid for several weeks. This effect can remain visible for several weeks and happens primarily because of the density of the steroid itself, as well as the translucence of the thin eyelid skin. Sometimes, this residual steroid is misdiagnosed as a side effect of injectable triamcinolone: depigmentation of the skin. In any case, the patient should be forewarned and educated about this possibility.
Some chalazia, especially those in the initial stages, are very soft, and the affected meibomian gland is not fully distended. This situation lends itself to a direct intralesional injection of the steroid. However, even in these situations, there still is not much physical space inside the meibomian gland to deposit much steroid. So, it is not critical that the injection be made intralesionally; paralesional injections work just as well.

When considering an injectable steroid for an eyelid “stye,” make sure that the condition is in fact a chalazion and not something else.
From a safety perspective, when eyelid steroid injections are made, it is important to keep the needle tip moving, and not remain stationary in one space. So, it is possible that one injection of the steroid, made in a translesional approach, can encompass both an intralesional and a paralesional injection.
Subconjunctival and Sub-Tenon’s injections
The indications for these types of injections often overlap; while the techniques for administering these injections are similar in approach, they are fundamentally different.
As the names indicate, the injected medication ultimately is delivered to either the subconjunctival space or the sub-Tenon’s space. Access to the subconjunctival space is easier than the sub-Tenon’s space. Also, given that the subconjunctival space is more anterior that the sub-Tenon’s space, subconjunctival injections have a more pronounced effect in the anterior segment, while sub-Tenon’s injections have more of an effect on
the posterior segment.8,9 In some situations, administering a subconjunctival injection of lidocaine prepares the tissue for a subsequent sub-Tenon’s injection.9
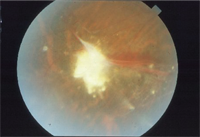
Uveitis, such as this
inflammatory chorioretinitis, may require steroid injection administered
to the sub-Tenon space or intravitreally.
Both types of injections are used primarily for the treatment of inflammation. Chronic, recalcitrant anterior uveitis can often be supplementally managed with a subconjunctival injection of steroid.8,9 It is important to note that when considering a subconjunctival injection of a steroid to facilitate control of recalcitrant uveitis, the patient must first demonstrate poor or minimal response to aggressive topical therapy.
In other words, subconjunctival steroid injections should not be used unless aggressive topical therapy with cycloplegics and topical steroids fail to control the anterior segment inflammation.
Also, subconjunctival steroid injections are not to be used in lieu of topical therapy, but used as adjunctive therapy along with the topical medications. Sub-Tenon’s injections are used to treat inflammations of the posterior segment, although with the advent of safer delivery systems and medications, intravitreal injections are also frequently used.
Intravitreal Injections
While these injections are not used by many optometrists, retinologists use them regularly in modern practice. Intravitreal injections are used to treat posterior segment disorders––mainly those of the macula. Given that the vitreous is avascular, absorption of intravitreously administered drugs is usually slow.
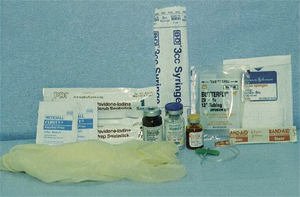
Common Supplies Needed for Injections
• Syringes, usually 1cc to 3cc
• Needles, usually 27ga to 30ga 3/8” to 5/8” for
periocular, 23ga 1.5” for extremity IM (insulin or
TB syringes work well for periocular injections)
• Alcohol wipes
• Adhesive bandages
• Sterile swabs
• Topical anesthetics
• Topical antibiotic drops and ointments
• Medication ampules or vials
• Forceps
• Lid speculum
Last but not least: Informed consent document
Angiogenic age-related macular degeneration is characterized by increased fluid accumulation in the subretinal space and/or in the intraretinal spaces. There are a variety of forms of wet AMD, but all are predicated upon the breakdown of the blood retinal barrier and the development of new blood vessels originating in the choroid. Anti-VEGF therapy targets certain growth factors that are responsible for the genesis of neovascular membranes, which are susceptible to leakage and hemorrhage; this is the basis of vision loss in patients with angiogenic AMD.
When administered into the vitreous cavity, anti-VEGF agents are in close proximity to the neovascular membranes, and produce fewer systemic side effects than if given by other routes of administration. Lucentis (ranibizumab, Genentech) and off-label Avastin (bevacizumab, Genentech) are prime examples of anti-VEGF medications that are administered by intravitreal injection.
Steroids such as Kenalog are also administered intravitreally, although for different reasons. Macular edema—whether from diabetic maculopathy, vein occlusions or other non-angiogenic diseases where fluid accumulates in the central macula and threatens vision—has been found to respond to intravitreal Kenalog (IVK) administration. Though other treatments are often used in conjunction with IVK therapy (focal laser, for example), IVK remains a viable treatment option for many cases of macular degeneration.
Intravenous Injections
Intravenous (IV) injections are usually used only in diagnostic procedures in the context of ophthalmic care. Fluorescein angiography, indocyanine green angiography and, less frequently, Tensilon (edrophonium, Valeant Pharm.) testing are all performed with IV-administered drugs.
Both the advantage and disadvantage to IV injections lies in the almost instant absorption of the drug into the vascular system. Desired effects, such as being able to evaluate fluorescein flow through the eye, happen quickly. But, unwanted side effects also occur quickly and more noticeably when drugs are administered via the IV route.
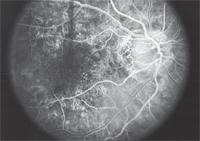
A prime example of intravenous (IV) administration in eye care: fluorescein angiography.
Intracameral Injections
These injections are usually reserved for operation room procedures during intraocular surgery. These would not be used in day-to-day clinical eye care.
The injectable route of administration is simply an alternative way to deliver medicine to the body. Injectable medications can be used as primary therapies and as adjunctive therapies. Being familiar with their indications and uses is imperative in current optometric practice.
Dr. Fanelli is in private practice in Wilmington, N.C., writes Review of Optometry’s “Glaucoma Grand Rounds” column, and lectures on glaucoma and other clinical topics.
1. Ison CA, Alexander S.
Antimicrobial resistance in Neisseria gonorrhoeae in the UK:
surveillance and management. Expert Rev Anti Infect Ther. 2011
Oct;9(10):867-76.
2. Carannante A, Prignano G, Cusini M, et al. Cefixime and ceftriaxone
susceptibility of Neisseria gonorrhoeae in Italy from 2006 to 2010. Clin
Microbiol Infect. 2011 Jun 28. doi: 10.1111/j.1469-0691.2011.03619.x.
[Epub ahead of print]
3. Roy FH, Fraunfelder FW, Fraunfelder FT. Roy and Fraunfelder’s Current
Ocular Therapy. 6th ed. Philadelphia: Saunders/Elsevier; 2008:32-33.
4. Darlington AB. The Botox phenomenon. Plast Surg Nurs. 2010 Jan-Mar;30(1):22-6.
5. Matarasso A, Shafer D. Botulinum neurotoxin type A-ABO (Dysport):
clinical indications and practice guide. Aesthet Surg J. 2009 Nov;29(6
Suppl):S72-9
6. Braccini F, Dohan Ehrenfest DM. Advantages of combined therapies in
cosmetic medicine for the treatment of face aging: botulinum toxin,
fillers and mesotherapy. Rev Laryngol Otol Rhinol (Bord).
2010;131(2):89-95.
7. Blumenfeld A,
Silberstein SD, Dodick DW, et al. Method of injection of
onabotulinumtoxinA for chronic migraine: a safe, well-tolerated, and
effective treatment paradigm based on the PREEMPT clinical program.
Headache. 2010 Oct;50(9):1406-18.
8. Kanski JJ, Bowling B. Clinical Ophthalmology: A Systematic Approach. 7th ed. Philadelphia: Saunders/Elsevier; 2011:411-12.
9. Ehlers JP, Chirag PS, Gregory LF, et al. The Wills Eye Manual: Office
and Emergency Room Diagnosis and Treatment of Eye Disease. 5th ed.
Philadelphia: Lippincott Williams & Wilkins; 2008:422.
| Authority of Optometrists to Administer Drugs Via Injection
| ||
| State
|
Use of Injectable Drugs for Diagnostic and Treatment Purposes 1 [including the treatment of anaphylaxis]
|
Use of Injectable Drugs Currently Limited to Treatment of Anaphylaxis Only
|
| Alaska
|
YES
|
|
| Alabama
|
|
YES
|
| Arizona
|
|
YES
|
| Arkansas
|
|
YES
|
| California
|
|
YES
|
| Colorado
|
|
YES
|
| Connecticut
|
|
YES
|
| D.C.
|
|
YES
|
| Hawaii
|
|
YES
|
| Idaho
|
YES
|
|
| Illinois
|
|
YES
|
| Iowa
|
|
YES
|
| Kentucky
|
YES
|
|
| Louisiana
|
|
YES
|
| Maine
|
|
YES
|
| Maryland
|
|
YES
|
| Minnesota
|
|
YES
|
| Mississippi
|
|
YES
|
| Montana
|
YES
|
|
| New Hampshire
|
|
YES
|
| New Jersey
|
|
YES
|
| New Mexico
|
YES
|
|
| North Carolina
|
YES
|
|
| North Dakota
|
YES
|
|
| Ohio
|
|
YES
|
| Oklahoma
|
YES
|
|
| Oregon
|
YES
|
|
| Tennessee
|
YES
|
|
| Texas
|
|
YES
|
| Utah
|
YES
|
|
| Vermont
|
|
YES
|
| Virginia
|
|
YES
|
| Washington
|
|
YES
|
| West Virginia
|
YES
|
|
| Wisconsin
|
YES
|
|
| ¹ The authority to administer injectable
drugs for diagnostic and treatment purposes may be limited by the state
optometry act or regulations.
Source: American Optometric Association State Government Relations Center | ||

