 |
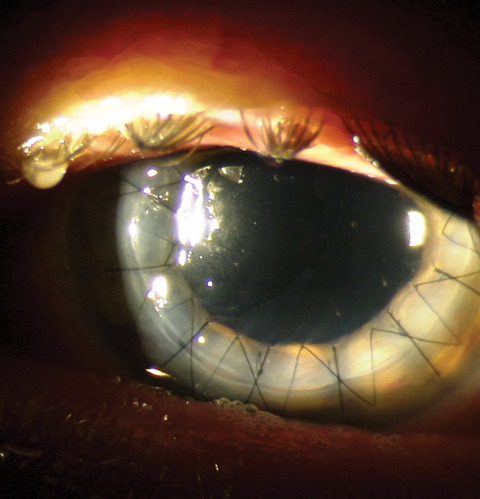
While infectious keratitis after keratoplasty is rare, the risk is increased fourfold in patients—especially elders—who undergo penetrating keratoplasty compared with endothelial keratoplasty. Photo: Mitch Ibach, OD. Click image to enlarge. |
Today, keratoplasty is the most performed transplant procedure in the US and has only become more popular over the last decade. Like any surgery, however, it doesn’t come without potential complications, the most important being infectious keratitis due to its sight-threatening potential. A recent retrospective cohort study evaluated the incidence of this complication following two types of keratoplasties—penetrating keratoplasty (PK) and endothelial keratoplasty (EK)—and found that patients who underwent the former had a fourfold increase in the likelihood of developing infectious keratitis within six months of the procedure.
The researchers identified a total of 115,588 keratoplasties (20% [23,144] PK and 80% [92,444] EK) performed on Medicare beneficiaries aged 65 years and older between 2011 and 2020. By six months post-op, infectious keratitis had developed in 3.32% of those who received PK and 0.72% of those who received EK. The researchers reported that the median interval between keratoplasty and infectious keratitis diagnosis was 73 days (ranging from 29 to 114 days) for PK and 74 days (ranging from 38 to 116 days) for EK. Roughly one-fifth of eyes that developed infectious keratitis underwent repeat keratoplasties within one year postoperatively (22.9% and 23.8% for PK and EK, respectively).
“The higher rates for infectious keratitis after PK compared with EK are expected because suture-related infections and impaired re-epithelialization are more likely with PK,” the study authors explained in their paper in Cornea. “Moreover, a larger proportion of indications for PK are higher risk (e.g., repeat keratoplasty or ectasias) relative to EK (e.g., endothelial dystrophy) as reported by the Eye Bank Association of America,” they added.
The researchers did find that the overall rates of infectious keratitis decreased between 2011 and 2020 from 16.05 to 9.61 per 1000 keratoplasties; however, this trend was determined to be due only to a reduction in post-EK infectious keratitis, while post-PK infection rates remained stable during this period.
Post-PK infectious keratitis was associated with age 85 years and older (odds ratio: 1.38) compared to those aged 65 to 74 years. Post-EK infectious keratitis was also associated with age 85 years and older (OR: 1.44) relative to the younger age group. The researchers reasoned in their paper that this finding “may relate to [the 85+ age group’s] overall health and limitations in complying with postoperative instructions.” To further support this rationale, they cited a multicenter cross-sectional study on 191,242 individuals in China, which “found that elderly patients have higher odds of developing infectious corneal blindness.” Because of this, the researchers argue, “Corneal surgeons should counsel elderly patients about the signs of infectious keratitis including pain, redness, and decreased vision and potentially schedule more frequent follow-ups for surveillance.”
The team concluded from their findings that “infectious keratitis was four times more common after PK than EK, and the complication was associated with older age. Our findings may help corneal surgeons in counseling patients at higher risk and guiding their postoperative care,” they wrote in their paper.
Muhammad A, Chen D, Kyongjin C, et al. Infectious keratitis after keratoplasty in the United States: analysis of a national Medicare claims data set. Cornea. October 30, 2023. [Epub ahead of print]. |

