 |
|
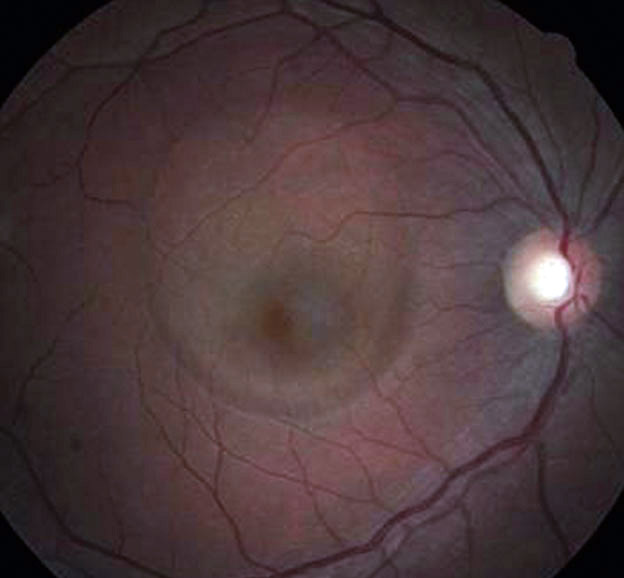
H. pylori infection treatment may be beneficial for CSCR patients due to the higher prevalence of this infection in these patients. One study cited in this review found that untreated patients with H. pylori infection had declining VA starting at six months and required six months for resorption of subretinal fluid. Also, recurrence rate was 52% for untreated patients vs. 6% in those who received therapy. Photo: Andrew S. Gurwood, OD. Click image to enlarge. |
Although a wide range of modalities have been proposed as therapeutics for central serous chorioretinopathy (CSCR), an expansive review of the safety and efficacy of these choices remains largely unexplored on a wider scale. Researchers aimed to help by conducting a literature search of multiple CSCR treatment modalities for a new Ophthalmic Technology Assessment by the American Academy of Ophthalmology. The paper was published in the Academy’s journal Ophthalmology on Tuesday.
The review yielded 612 citations, of which 31 were included for full review and inclusion in the assessment. Most studies were published within the last 15 years, but one paper dates back to 1983. Each study was given a level of evidence rating based on the panel methodologist’s assessment. This yielded six studies being assigned a level I rating, 23 deemed level II and two considered to be level III. Studies were categorized by treatment type, which included laser-based therapy, intravitreal therapy, laser-based therapy vs. intravitreal therapy and systemic therapies.
The researchers highlight in their paper the findings of level I evidence—the highest level achievable. One of these studies investigated photodynamic therapy using half-dose verteporfin for acute CSCR. It was found that this led to a significant decrease in subretinal fluid, as none was observed in 95% of patients treated with this option at 12 months, while this was only achieved in 58% of untreated eyes over the same time period. As well, the mean central foveal thickness was significantly lower at one year in the treated group (161µm ±65µm) vs. the untreated group (278µm ±92µm).
In another level I study, half-dose verteporfin photodynamic therapy was compared against a 30%-dose option. The findings in this investigation included 94.6% of those in the half-dose group with no subretinal fluid at 12 months; compare this with the lower 75.4% with no subretinal fluid at 12 months in the 30%-dose group. However, the noninferiority of the 30%-dose compared with half-dose was not demonstrated.
A study known as the VICI trial, also with level I evidence, found no benefit of using mineralocorticoid antagonist therapy with eplerenone (a diuretic) for chronic CSCR cases. The primary outcomes of the study was visual acuity, and no significant difference was found at 12 months, with the placebo group achieving, on average, 79.5 letters and the eplerenone group achieving 80.4 letters.
Although many other studies were included, the results in general were inconsistent and thus inconclusive. No level I studies supported a role for intravitreal anti-VEGF injections or systemic beta-blockers; however, there was one small level I study that displayed potential efficacy of Helicobacter pylori therapy. Looking at all studies included, many eyes with acute CSCR resolve spontaneously.
When considering clinical application of these findings, the authors of the study wrote that “there is evidence to support half-dose photodynamic therapy for the treatment of acute CSCR regarding anatomic improvement, but less robust evidence supports improvement in visual acuity or sustained anatomic benefit beyond 12 months.” The authors also remind readers that “many eyes with acute CSCR resolve spontaneously,” and thus intervention many not always be required.
| Click here for journal source. |
Kim LA, Maguire MG, Weng CY, et al. Therapies for central serous chorioretinopathy: a report by the American Academy of Ophthalmology. Ophthalmology. October 22, 2024. [Epub ahead of print]. |

