 |
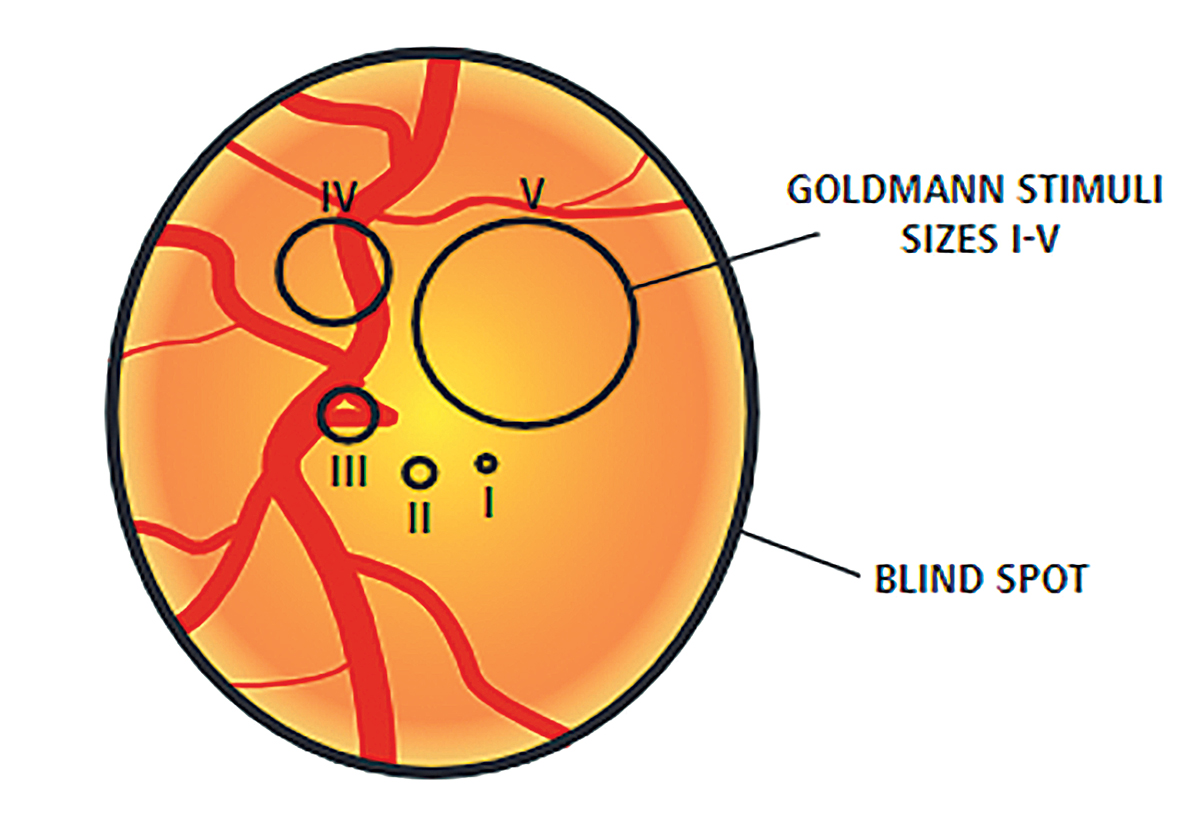
| Goldmann size II allowed for better correlations between VF data and the corresponding macular GCL thickness when evaluating the relationship between the less affected nasal VF and temporal macular parameters. Photo: Anders Heijl and Vincent Michael Patella. Click image to enlarge. |
With modern OCT equipment capable of providing detailed measurements of all retinal layers in the macula, many studies have found macular ganglion cell layer (GCL) abnormalities on OCT despite the absence of abnormalities in visual field (VF) tests using the standard Goldmann size III stimulus. Several authors have argued that SAP using the standard Goldmann size III stimulus is relatively insensitive at detecting early optic pathway damage from glaucoma and compressive optic neuropathies based on the observation that structural abnormalities (especially macular GCL loss) can precede the development of VF defects. Researchers in Brazil investigated which of the three Goldmann stimulus sizes was best able to discriminate between healthy controls and patients with subtle changes in the less-affected part of the VF due to compressive optic neuropathy and to determine the best correlation with macular GCL thickness. They determined that Goldmann sizes II and III were both efficient at distinguishing the groups, suggesting they are suitable for clinical evaluations of the central 10-2 VF.
A cross-sectional study was conducted involving 30 eyes from 25 patients with temporal VF loss on 24-2 SITA standard automated perimetry due to previous chiasmal compression and 30 healthy eyes (23 controls). Optical coherence tomography (OCT) of the macular area and 10-2 VF testing using Goldmann stimulus sizes I, II and III were performed in the Octopus 900 perimeter. Macular GCL thickness and VF data were segregated into four quadrants (two temporal and two nasal) and two halves (temporal and nasal) centered on the fovea to evaluate separately both the severely affected nasal hemi-retina corresponding to the temporal VF sectors and the subclinically affected temporal hemi-retina corresponding to the nasal VF sectors.
All macular GCL parameters in the nasal and temporal halves of the retina were significantly reduced in patients compared with controls. The researchers noted that 10-2 VF test sensitivity using Goldmann sizes I, II and III was significantly lower in patients than in controls for all parameters, except the three nasal divisions when using size I.
Significant correlations were found between temporal VF sectors (all stimulus sizes) and the corresponding nasal macular GCL measurements, with similar discrimination ability. Significant correlations were also observed between all three nasal VF divisions and the corresponding temporal macular GCL thickness when using stimulus sizes I and II but not stimulus size III.
“Our findings suggest that GI is inadequate for this analysis as it leads to greater response variability and consequently diminishes the ability of the test to differentiate healthy controls from patients previously treated for chiasmal compression,” the authors wrote in their paper.
In addition to the classical temporal hemianopic field defect and its corresponding retinal structural damage, the nasal VF sectors and temporal macular ganglion cell layer thickness can also be affected by chiasm compressive lesion, even though the VF tests with size III stimulus are described as “within normal limits” by the equipment database.
Rocha AADN, Benassi TSA, Mello LGM, et al. Discrimination ability of central visual field testing using stimulus size I, II and III and relationship between VF findings and macular ganglion cell thickness in chiasmal compression. PLoS One. 2024;19(3):e0300103. |

