 |
Q: Can corneal hysteresis (CH) aid intraocular pressure (IOP) assessment in keratoconus (KCN)?
A: “Hysteresis is a measurement characterizing how something responds to the loading and unloading of an applied force,” says Paymaun Asnaashari, OD, who practices in northern California. “It is not a constant property, like thickness or weight, but a measurement that is dependent on the elastic properties and viscosity of a material or system.” The cornea is a viscoelastic tissue, and CH reflects its ability to absorb and dissipate energy.1
Discussion
There is growing evidence regarding CH and its relationship to optic nerve changes, but the exact mechanism of how a lower CH may contribute to development or progression of glaucoma still remains unclear, as the intrinsic properties of the eye that CH aims to measure are not well understood, Dr. Asnaashari says.
However, study findings support the hypothesis that CH serves as a surrogate biomarker of the viscoelastic properties of the lamina cribrosa, posterior sclera and other optic nerve structures.2 The idea that a lower CH is associated with lower optic nerve biomechanical rigidity supports the theory that it can lead to posterior displacement of the lamina cribrosa, he notes. A lower CH may indicate a decreased ability of the posterior tissues to compensate for IOP changes.2 An association between lower CH and higher vertical c/d ratios with optic disc hemorrhages has also been reported.3 This suggests the biomechanical properties of the cornea are important in glaucomatous optic changes.
 |
|
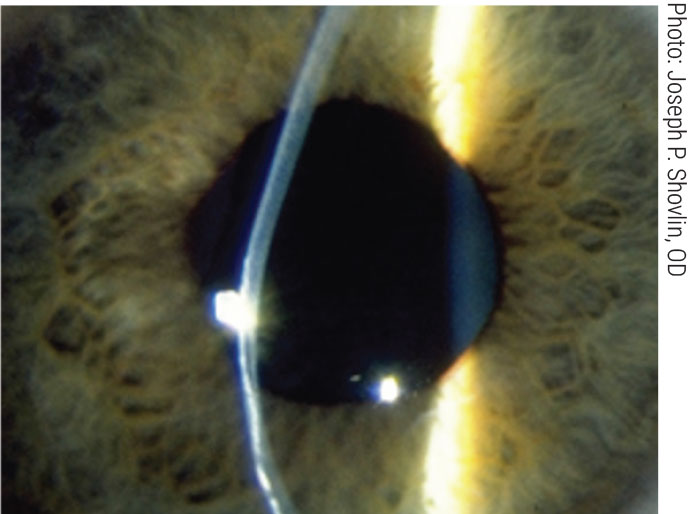
Studies have observed lower CH in KCN, which may be an indicator for glaucoma risk. Click image to enlarge. |
CH has been shown to be lower in glaucoma, with studies demonstrating that a lower CH is a risk factor for visual field progression and retinal nerve fiber layer thinning.4-8 Accordingly, patients with a higher CH may not exhibit the same IOP-lowering effects across the same therapies—pressure reduction in a patient with a high CH may be significantly less.9
It can be tempting to start a patient on a second drop if their IOP does not reach its target, but if the patient has a high CH, we can expect a lower risk of progression and less of an effect on IOP. Another study showed further evidence of an inverse association between CH and magnitude of IOP reduction post-MIGS.10 Within the same study, there was an increased need for repeat surgeries or other interventions for patients with a lower CH.10
Multiple studies have found that CH is lower in KCN eyes and that the measurement decreases with increasing corneal steepening and thinning as the disease becomes more severe.4,11,12 It has been supported that CH also naturally drops with age.13 Other studies have suggested that the LASIK flap creation and corneal thinning weaken the cornea and reduce CH, potentially leading to the development of new parameters for screening candidates for refractive surgery.14,15 However, it is not yet supported that patients with corneal ectasia disease who are glaucoma patients or suspects have a lower CH than patients with corneal ectasia disease alone.16
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
1. Deol M, Taylor DA, Radcliffe NM. Corneal hysteresis and its relevance to glaucoma. Curr Opin Ophthalmol. 2015;26(2):96-102. 2. Ortiz D, Piñero D, Shabayek MH, et al. Corneal biomechanical properties in normal, post-laser in situ keratomileusis, and keratoconic eyes. J Cataract Refract Surg. 2007;33(8):1371-5. 3. Radcliffe NM, Tracer N, De Moraes CGV, et al. Relationship between optic disc hemorrhage and corneal hysteresis. Can J Ophthalmol. 2020;55(3):239-44. 4. Congdon NG, Broman AT, Bandeen-Roche K, et al. Central corneal thickness and corneal hysteresis associated with glaucoma damage. Am J Ophthalmol. 2006;141(5):868-75. 5. Kamiya K, Miyata K, Tokunaga T, et al. Structural analysis of the cornea using scanning-slit corneal topography in eyes undergoing excimer laser refractive surgery. Cornea. 2004;23(8 Suppl):S59-64. 6. Jaycock PD, Lobo L, Ibrahim J, et al. Interferometric technique to measure biomechanical changes in the cornea induced by refractive surgery. J Cataract Refract Surg. 2005;31(1):175-84. 7. Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):714-20. 8. Abitbol O, Bouden J, Doan S, et al. Corneal hysteresis measured with the Ocular Response Analyzer in normal and glaucomatous eyes. Acta Ophthalmol. 2010;88(1):116-9. 9. Agarwal DR, Ehrlich JR, Shimmyo M, et al. The relationship between corneal hysteresis and the magnitude of intraocular pressure reduction with topical prostaglandin therapy. Br J Ophthalmol. 2012;96(2):254-7. 10. Tracer N, Ayoub S, Radcliffe NM. The association between corneal hysteresis and surgical outcomes from trabecular meshwork microinvasive glaucoma surgery. Graefes Arch Clin Exp Ophthalmol. 2021;259(2):475-81. 11. Anand A, De Moraes CGV, Teng CC, et al. Corneal hysteresis and visual field asymmetry in open angle glaucoma. Invest Ophthalmol Vis Sci. 2010;51(12):6514-8. 12. Medeiros FA, Meira-Freitas D, Lisboa R, et al. Corneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal study. Ophthalmology. 2013;120(8):1533-40. 13. Sharifipour F, Panahi-Bazaz M, Bidar R, et al. Age-related variations in corneal biomechanical properties. J Curr Ophthalmol. 2016;28(3):117-22. 14. Zhang C, Tatham AJ, Abe RY, et al. Corneal hysteresis and progressive retinal nerve fiber layer loss in glaucoma. Am J Ophthalmol. 2016;166:29-36. 15. Cohen EJ. Keratoconus and normal-tension glaucoma: a study of the possible association with abnormal biomechanical properties as measured by corneal hysteresis. Trans Am Ophthalmol Soc. 2009;107:282-99. 16. Wong BJ, Moghimi S, Zangwill LM, et al. Relationship of corneal hysteresis and anterior lamina cribrosa displacement in glaucoma. Am J Ophthalmol. 2020;212:134-43. |

