 |
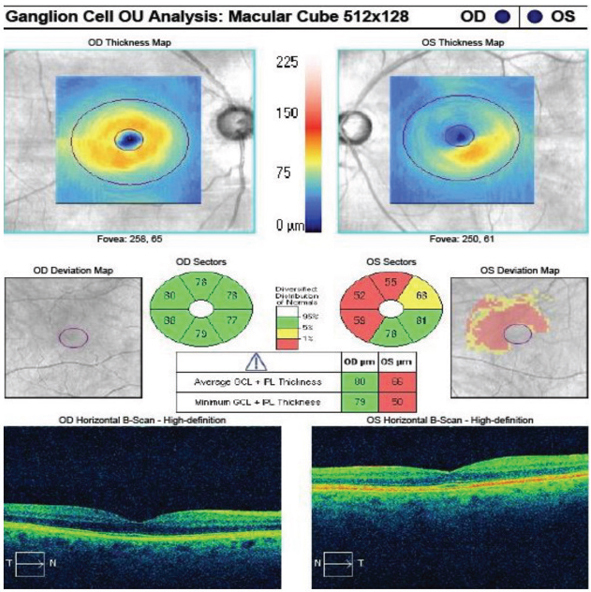
| The lack of difference in average GCC thickness between early AMD and intermediate AMD eyes suggests to researchers that substantial inner retinal changes occur in the transition from normal aging to late AMD, with minimal variance between early and intermediate stages. This GCC scan is from a glaucoma patient not involved with this study. Photo: Brian Fisher, OD. Click image to enlarge. |
While age-related macular degeneration (AMD) primarily affects the outer retinal layers, recent studies have shown alterations in the inner retinal layers including the ganglion cell complex (GCC), which comprises the ganglion cell layer (GCL), inner plexiform layer and retinal nerve fiber layer. One recent investigation reported significant GCL thinning in the fellow eyes of patients with macular neovascularization (MNV) vs. age-matched controls. Another found a strong correlation between GCC thickness and photoreceptors normalized reflectivity in eyes with intermediate AMD. Additionally, histopathological studies have shown that post-mortem eyes with MNV have 47% fewer GCL neurons than healthy eyes.
Researchers of a new post-hoc analysis in American Journal of Ophthalmology pointed out that one limitation of these prior investigations is the heritability of GCC thickness. “Studies have suggested that additive genetic factors are responsible for 81% of the variance in age-adjusted thickness, while environmental factors account for the three remaining 19% of the variance,” the study authors wrote in their paper. “The use of a relatively isolated population can mitigate some of these concerns.” Thus, the team recruited subjects from three Amish communities, known for their genetic and cultural isolation, who were enrolled in the Amish eye study and compared GCC thickness between those with and without AMD.
All participants were imaged by the Cirrus HD-OCT (Carl Zeiss Meditec) using a macular cube protocol of 512 x 128 scans (128 horizontal B-scans, each compromising 512 A-scans) over a 6mm x 6mm region centered on the fovea. Of 1,339 subjects in the Amish eye study, 1,294 eyes of 1,294 subjects (62% female) had sufficient-quality images and were included in the final analysis.
Even after adjusting for age, the average GCC thickness was significantly thinner in eyes with AMD (73.7µm ± 13.8µm) compared to normal eyes (78.0µm ± 10.42µm). There were also some noted differences in GCC thickness among the different stages of AMD; eyes with early or late AMD showed a statistically significant lower GCC thickness compared to eyes without AMD. Late AMD eyes, particularly those with geographic atrophy (GA), had the lowest GCC thickness (58.1µm ± 20.3µm).
Interestingly, there was no significant difference in average GCC thickness between early AMD and intermediate AMD eyes, which the researchers note suggests that “there may be subtle but significant alterations in the inner retina in the transition from normal aging to early AMD, but substantial changes do not occur until the disease progresses to the late stage.”
Regarding the gender variable, no differences were noted in GCC thickness between males and females for any AMD group.
Overall, this study demonstrates that GCC thickness is reduced in AMD eyes, with the greatest reduction observed in late AMD eyes, particularly those with geographic atrophy. “Future therapeutic strategies for AMD may need to consider these inner retinal alterations and their potential impact on response to therapy,” the researchers concluded.
Velaga S, Algore A, Mehedi M, et al. Alterations of the ganglion cell complex thickness in age-related macular degeneration: an AMISH Eye Study analysis. Am J Ophthalmol. April 25, 2024. [Epub ahead of print]. |

