 |
Q:
I have seen several post-op cataract patients who complain of blacking out of vision when going from a sitting to standing position. The eye looks fine. What is going on?
“Intraocular pressure (IOP) change after cataract surgery is a commonly seen postoperative complication that can manifest in several different ways,” says Himakshi Bhatt, OD, of Ophthalmic Consultants of Connecticut in Fairfield, CT. “Fortunately, these events can be easily handled in office by any comanaging doctor.”
Elevated IOP the day after surgery is often caused by residual viscoelastic in the trabecular meshwork. Corneal signs include microcystic epithelial edema and stromal folds. If IOP is lower than average, note anterior chamber depth and check for a seidel at the incision sites. Patients are often asymptomatic with low IOPs or if IOPs have increased into the 20s. However, once pressure starts creeping into the 30s and 40s, patients may start complaining of headaches and eye aches, as well as blurred or hazy vision.
Infrequently, patients may complain of blacking out of vision in the surgical eye, as described by this patient. This interesting finding is most likely related to perfusion pressure at the optic nerve head. Dr. Bhatt had two similar cases recently. Both patients were women in their 50s with low blood pressures and elevated IOPs. One woman had pressures in the high 30s and the other in the mid 20s. They experienced momentary blacking out of vision in the operative eye when going from a sitting to a standing position. All slit lamp and dilated fundus exam findings were unremarkable besides the elevated IOP. In both cases, symptoms completely resolved once IOPs reached a normotensive level.
 |
|
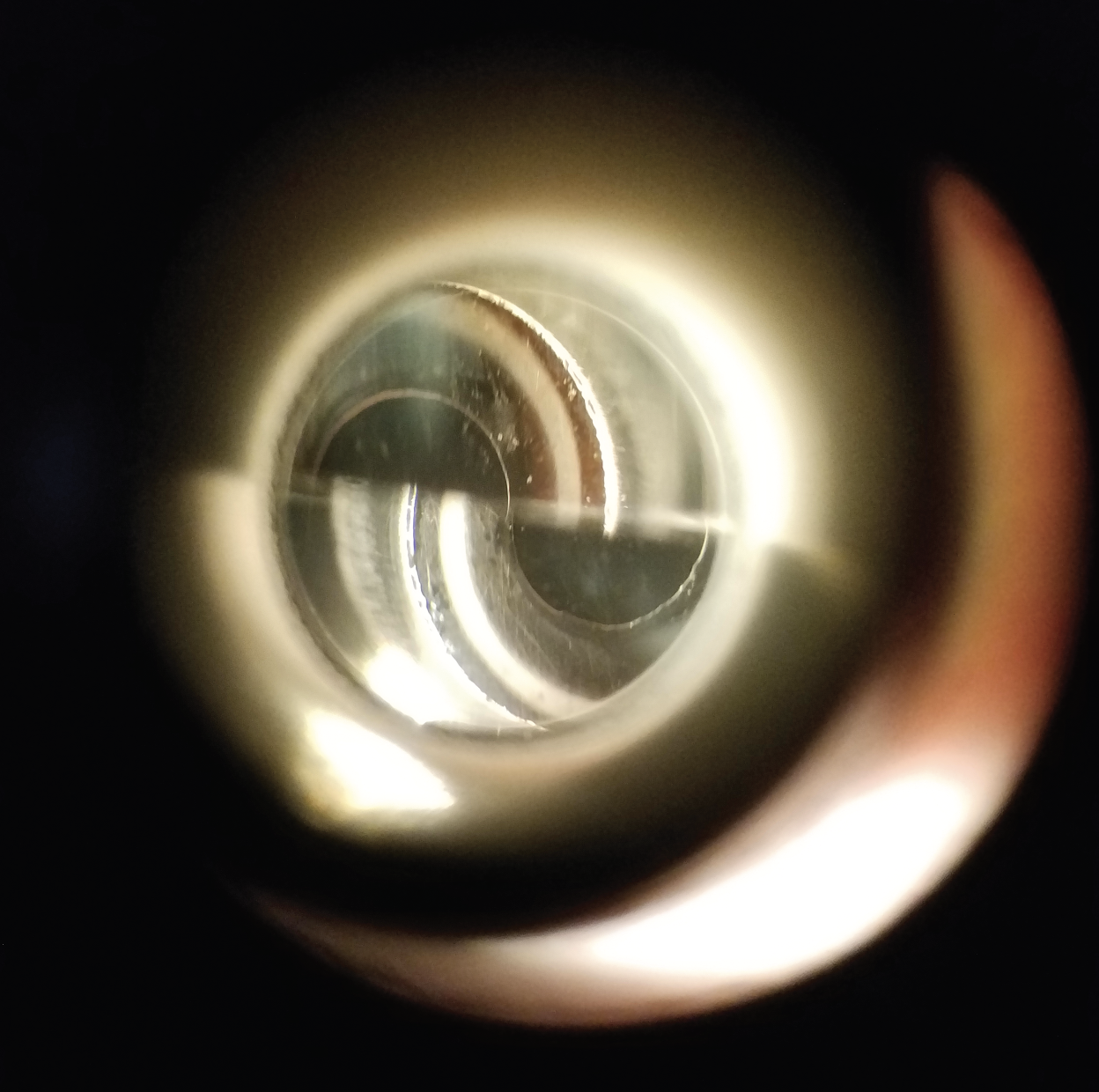
Transient post-surgical elevated IOP can be easily managed with topical hypotensive therapy. Click image to enlarge. |
A Rush of Blood
To understand the mechanism of action for this unique surgical complication, it is important to review optic nerve head blood supply and vasculature. The optic nerve head is supplied by the posterior ciliary arteries, which branch from the ophthalmic artery.1 Blood returns from the nerve head and peripapillary region via the central retinal vein.1 Ocular perfusion pressure (OPP) is the difference between atrial and venous blood pressure and is the pressure at which blood enters the eye.1,2 Atrial pressure pushes blood into the eye while IOP pushes blood out. The balance between these two determines blood supply and oxygen delivery to the optic nerve and retinal ganglion cells. OPP is low when systemic blood pressure is low, when IOP is high or both.2,3
Blood supply to cerebral structures can be affected by positional changes. When going from sitting or supine to standing, there is a sudden reduction in arterial blood pressure, as body fluid pools in the legs and lower body.4 This momentary and sudden drop in blood flow to the head is highlighted in patients with orthostatic hypotension or orthostatic intolerance.4 Women may be more prone to the effects of this postural change vs. men.4
“Adding together the patients’ low blood pressure and reduced blood supply caused by a positional change, along with an increased IOP, it creates the perfect storm for reduced ocular perfusion, and therefore transient vision loss as seen in the cases described above,” Dr. Bhatt says. “When IOP returns to normal levels, this balance is restored and the vision change is resolved. A proper work-up should be performed for any patient complaining of repeated temporary vision loss, or amaurosis fugax.”
“Elevated IOP is an easily managed complication after cataract surgery, but may present in more than just one way,” she emphasizes. “Take care of IOP in the 30s with drops and 40s by burping the wound. Then, make sure you measure their blood pressure.”
Dr. Ajamian is board certified by the American Board of Optometry and serves as Center Director of Omni Eye Services of Atlanta. He is vice president of the Georgia State Board of Optometry and general CE chairman of SECO International. He has no financial interests to disclose.
1. Mackenzie PJ, Cioffi GA. Vascular anatomy of the optic nerve head. Can J Ophthalmol. 2008;43(3):308-12. 2. Cherecheanu AP, Garhofer G, Schmidl D, et al. Ocular perfusion pressure and ocular blood flow in glaucoma. Curr Opin Pharmacol. 2013;13(1):36-42. 3. Kim KE, Oh S, Baek SU, et al. Ocular perfusion pressure and the risk of open-angle glaucoma: systematic review and meta-analysis. Sci Rep. 2020;10(1):10056. 4. Patel K, Rössler A, Lackner HK, et al. Effect of postural changes on cardiovascular parameters across gender. Medicine (Baltimore). 2016;95(28):e4149. |

