 |
Corneal arcus is a regularly encountered condition on routine ophthalmic examination, as it is one of the most common ocular manifestations of aging. While this ubiquitous finding is most often benign, there are a few circumstances in which the practitioner should pause and consider a potentially life-threatening systemic etiology. In order to distinguish between these possibilities, it is necessary to understand what comprises a normal case of corneal arcus and how to identify atypical manifestations.
Squaring the Circle
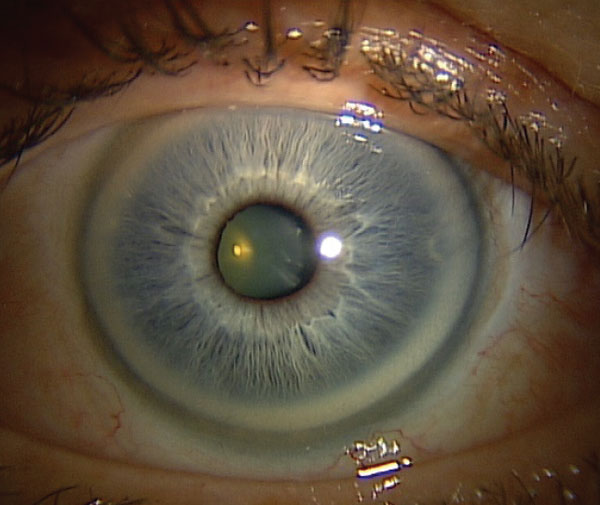
Corneal arcus appears as a bilateral, white or grey opacification encircling the cornea. There is a 1mm clear zone known as the lucid interval of Vogt between the opacification and the limbus that distinguishes the condition from other peripheral corneal degenerations.1,2 Corneal arcus usually begins to form around 6 or 12 o’clock and spreads until it comprises a full circle.2 Histopathological studies have reported that corneal arcus is an accumulation of cholesterol, phospholipids and triglycerides from the systemic circulation that is then deposited near the limbus at the level of the stroma, Bowman’s membrane and Descemet’s membrane.1,3,4
|
|
Age-related deposition of cholesterol and other lipids in the stroma occurs in response to increased permeability of the limbal blood vessels. Click image to enlarge. |
It is unclear why the lipid deposition is limited to a circular peripheral ring around the cornea. It could be that due to the cornea’s avascularity, the limbal blood vessels deposit material only on the outer regions. It has also been speculated that the temperature gradient of the cornea affects how lipids are deposited. Additionally, the precise arrangement of collagen and molecules within the corneal layers prohibits the movement of lipids into the center of the cornea.2
In elderly patients, corneal arcus is usually benign, without visual consequences or ocular complications. It is more commonly found in men than women and is also thicker and denser in appearance in men.1 Its incidence rises with age due to the increase in permeability of the limbal blood vessels with aging, allowing for easier lipid deposition from the bloodstream.4
As the condition is associated with normal aging and usually not considered pathologic in the elderly population, it may be indicative of abnormal lipid metabolism if identified in non-elderly patients.5 In the event that a middle-aged or younger patient presents with corneal arcus, studies have indicated a potential correlation with systemic hypercholesterolemia, specifically low-density lipoprotein build-up, and coronary artery disease.1
Corneal arcus arising in patients under 50 years of age, also known as arcus juvenilis, is a marker for lipid dysfunction and often yields chronically elevated serum cholesterol. It is estimated that males younger than 50 with arcus have a 6.4x higher risk of developing cardiovascular disease-related mortality. Treatment with a statin to lower cholesterol levels has been shown to result in a significant decrease in risk, though corneal findings remain unchanged.5 One study suggested a possible correlation between arcus and alcoholism in males under 60 years of age.6
|
|
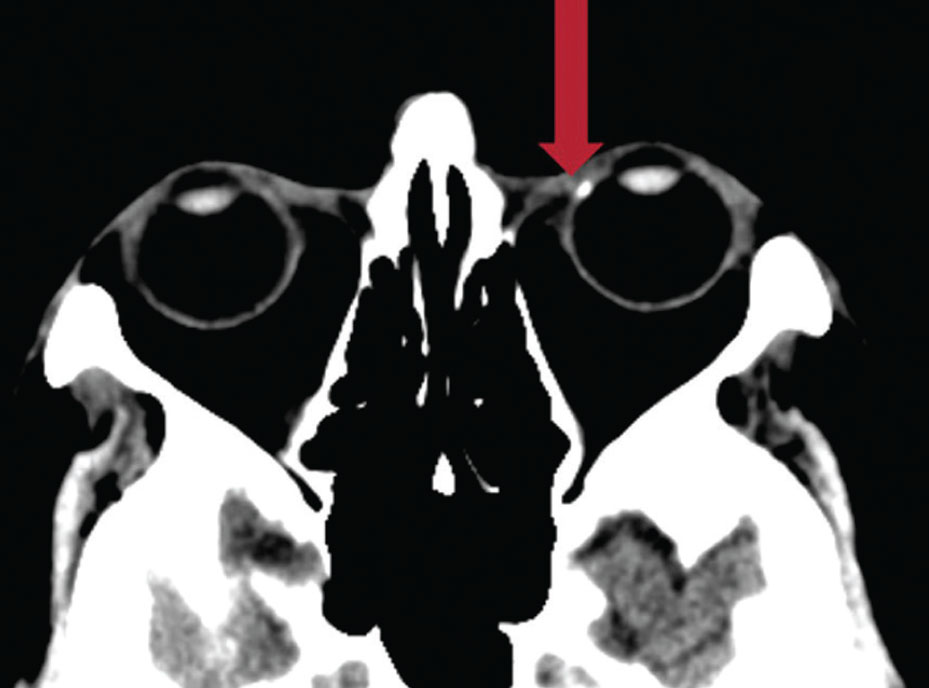
Corneal arcus appears hyper-dense on CT scans (red arrow). Click image to enlarge. |
In rare cases, arcus may be a unilateral finding. Some studies report that this is due to severe carotid occlusive disease, with arcus presenting only in the contralateral eye. This suggests that in the event there is a large, unilateral carotid plaque, the lack of blood flow prohibits arcus formation in the ipsilateral eye, while it is not restricted in the contralateral eye with patent carotid.7
The presence of arcus can have ocular implications as well as the aforementioned systemic risks. Ocular conditions such as chronic hypotony may also lead to a unilateral or asymmetric presentation of arcus. In this case, however, the arcus is present or more pronounced in the affected eye. This is likely due to the fact that the inflammatory process associated with the breakdown seen in ocular hypotony leads to increased vessel permeability and increased likelihood of lipid deposition from the bloodstream.8
Studies have considered the effect of arcus on the overall corneal composition and how it may affect the structure as it relates to measuring intraocular pressure (IOP) and hysteresis. It has been suggested that corneal hysteresis and resistance is lower in eyes with arcus when compared with eyes without.9 Furthermore, a study evaluating central corneal thickness (CCT) and IOP measurements demonstrated that, on average, eyes with arcus had lower CCT and higher IOP but not glaucoma. It is unclear what the cause of these associations is, but this finding suggests that the presence of arcus has an effect on the overall biochemical properties of the cornea.10
Takeaways
For most optometrists, there is rarely a clinical day that goes by where corneal arcus is not an encountered condition among our patients. Although it is most often a completely benign, age-related finding, all ODs should be aware of its atypical variants, as they may be more ominous. It is necessary to recognize these as the first signs of what could be a serious underlying health condition that requires intervention.
Dr. Labib graduated from Pennsylvania College of Optometry, where she now works as an associate professor. She completed her residency in primary care/ocular disease and is a fellow of the American Academy of Optometry and a diplomate in the Comprehensive Eye Care section. She has no financial interests to disclose.
1. Pe’er J, Vidaurri J, Halfon ST, et al. Association between corneal arcus and some of the risk factors for coronary artery disease. Br J Ophthalmol. 1983;67(12):795-8. 2. Zech LA Jr, Hoeg JM. Correlating corneal arcus with atherosclerosis in familial hypercholesterolemia. Lipids Health Dis. 2008;7:7. 3. Cooke NT. Significance of arcus senilis in Caucasians. J R Soc Med. 1981;74(3):201-4. 4. Raj KM, Reddy PAS, Kumar VC. Significance of corneal arcus. J Pharm Bioallied Sci. 2015;7(Suppl 1):S14-5. 5. Ang SM, Williams BK, Shields CL. Rings on the eyes, matters of the heart. Indian J Ophthalmol. 2018;66(4):494. 6. Ewing JA, Rouse BA. Corneal arcus as a sign of possible alcoholism. Alcohol Clin Exp Res. 1980;4(1):104-6. 7. Bagla SK, Golden RL. Unilateral arcus corneae senilis and carotid occlusive disease. JAMA. 1975;233(5):450. 8. Barchiesi BJ, Eckel RH, Ellis PP. The cornea and disorders of lipid metabolism. Surv Ophthalmol. 1991;36(1):1-22. 9. Ayhan Z, Ozturk T, Kaya M, et al. Corneal biomechanical properties in patients with arcus senilis. Cornea. 2016;35(7):980-2. 10. Wu R, Wong TY, Saw SM, et al. Effect of corneal arcus on central corneal thickness, intraocular pressure, and primary open-angle glaucoma: the Singapore Malay Eye Study. Arch Ophthalmol. 2010;128(11):1455-61. |

