 |
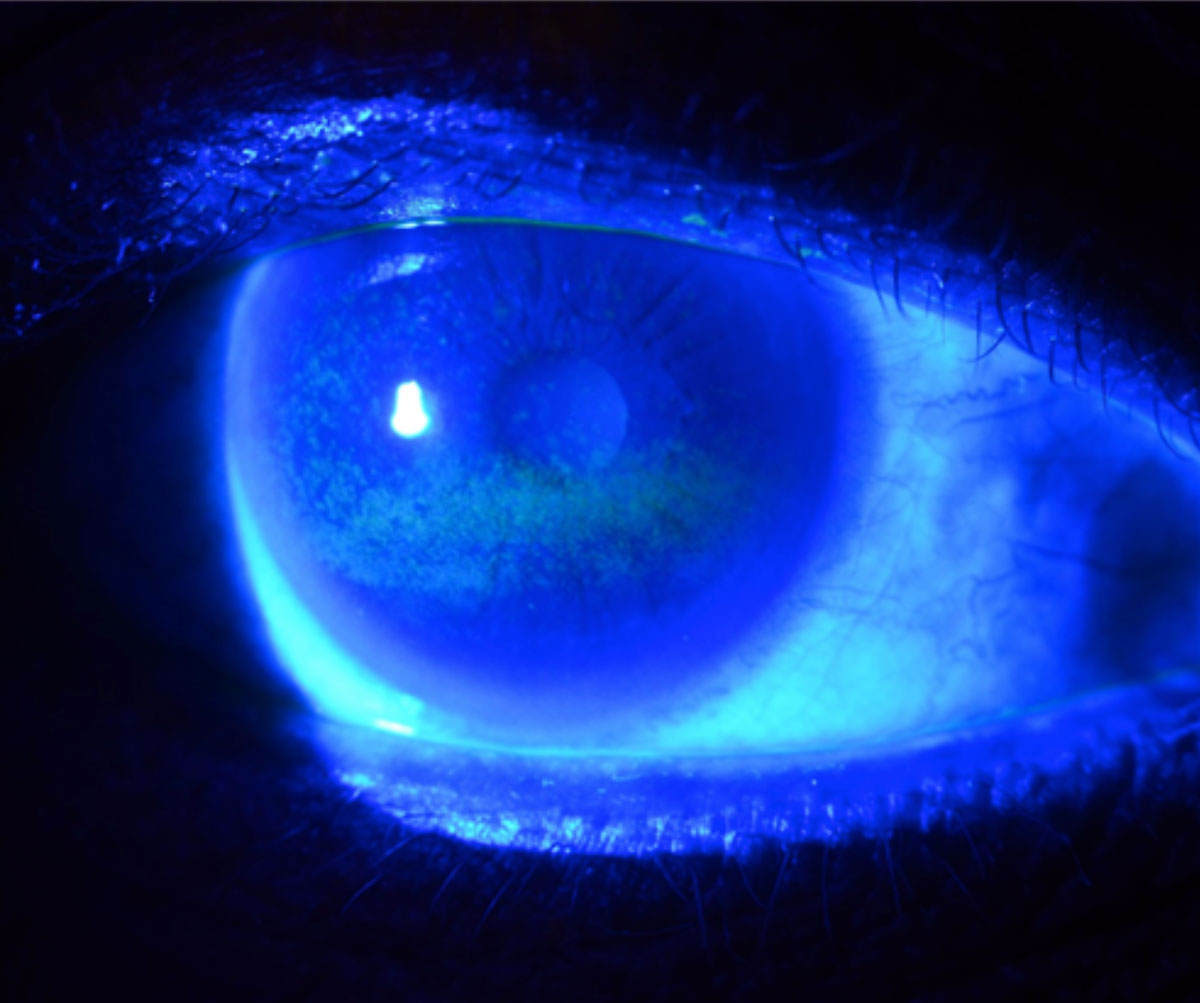
| Corneal staining was the most commonly used clinical sign in FDA trials of dry eye drugs, but even this metric was only used in six of 12 studies evaluated. Furthermore, the grading systems used for staining assessment varied from study to study. Photo: W.R. Buie, OD. Click image to enlarge. |
Ocular surface disease is widespread, estimated to affect anywhere from 5% to 50% of the global population, and is associated with various adverse health effects. Consequently, many topical therapies have been developed to help reduce or cure the condition. Researchers of a recent study were interested in investigating the clinical trial methodology of those treatments submitted to the FDA for approval and found considerable heterogeneity, prompting concerns about their applicability to daily practice.
Included in the analysis were 14 trials, with information collected about each study, patient demographics, treatment names and doses, sample size in each arm and measurement system. Five topical treatments were assessed across the trials, including cyclosporine 0.05%, cyclosporine 0.09%, lifitegrast 5% and loteprednol 0.25% eye drops and varenicline 0.03mg nasal spray. Treatment duration ranged from two to 24 weeks, on average taking place for 12 weeks. All trials, even with varying concentrations of the same treatment, were compared with vehicle.
Primary clinical signs were measured in 12 trials (85.7%) and 10 (71.4%) evaluated a primary patient-reported symptom. The most frequently evaluated clinical sign primary outcome was corneal staining, seen in six of 12 trials and was graded using four different scoring systems. Two different scoring systems were used each for conjunctival staining, conjunctival hyperemia and tear production. The only patient-reported symptom primary outcome was ocular discomfort, which was measured using five different instruments.
In their discussion, the authors relay that none of these trials were compared with artificial tears or a previously approved dry eye treatment; instead, all used the test drug’s vehicle. Artificial tears are an established first-line therapy for dry eye and are affordable, accessible over-the-counter and effective in most patients, making them the de facto baseline therapy that an investigational drug should be tested against for a more realistic appraisal of the clinical gain from a change in therapy, the authors argue in their paper for American Journal of Ophthalmology. They also point out that retina and glaucoma drugs are commonly tested for noninferiority to one of the current leading medications in the same class, a model future dry eye trials would do well to emulate.
A previous analysis noted that in 138 trials, 105 unique outcomes were measured with dry eye, and this is echoed in the findings here, too. The authors note that “the use of multiple clinical signs to evaluate dry eye severity highlights the absence of an agreed-upon physician measured sign to assess and monitor dry eye. This presents a barrier to evaluating the efficacy of prescription dry eye treatments in the clinical setting.” To solve this, they recommend corneal staining as an outcome with dry eye treatment, given clinical correlation with ocular inflammation and direct visual function impact.
Finally, patient demographics were limited, primarily consisting of older, non-Hispanic white females. Those who are younger, male, and racial and ethnic minorities were all sparse, prompting the researchers to highlight that “the efficacy of FDA-approved treatments for dry eye in underrepresented patient populations remains unclear and merits further research.”
Moving forward, the authors would like to add consistency to how these topical dry eye treatments are evaluated: “Clinically meaningful dry eye outcome measures and standardized measurements can optimize the assessment of and comparison of therapeutic benefits,” they wrote.
Cui D, Saldanha IJ, Li G, et al. United States regulatory approval of topical treatments for dry eye. Am J Ophthalmol. October 2, 2023. [Epub ahead of print]. |

