Q. Should I refer a patient with moderate to severe dry eye for LASIK?

A. There are varying opinions on the subject of LASIK for dry eye patients. In general, LASIK in severe dry eye patients should be avoided, says optometrist Richard Phillips, Regional Clinical Director/Advisor for TLC Laser Eye Centers. Slit lamp assessment with staining agents, TBUT (tear-break-up-time) and evaluation of the lacrimal lake are the best means of evaluating a patients potential candidacy for LASIK, he says.
Patients with a TBUT of less than 10 seconds should be evaluated further to determine whether punctal plugs are necessary, or if the patient should not undergo LASIK. Says Dr. Phillips: Most patients with moderate dry eye complaints will have good results with punctal occlusion, compliant artificial tear treatment and occasionally, cyclosporine therapy.
Tear film stability analysis may be a useful means of screening LASIK candidates for dry eye prior to surgery. It may also help define dry eye symptoms after. A study published last month in the American Journal of Ophthalmol-ogy used new videokeratography software for a topographic modeling system. The system can automatically capture consecutive corneal surface images every second for ten seconds. Thirty-four subjects who underwent myopic LASIK were evaluated before surgery, at 1 week, 1 month, 3 months and 6 months after surgery. Subjects with abnormal tear film stability were more likely to develop superficial punctate keratitis (SPK) and also displayed resistance to dry eye treatment. This correlated well with the patients pre-surgical tear-film analysis, leading the researchers to conclude this tool is valuable in predicting dry eye problems post-LASIK.1
Severe dry eye patients simply should not undergo LASIK. LASIK is contraindicated in patients with complex dry eye syndrome from lacrimal insufficiency. One study compares the effects of corneal hydration during LASIK by blotting the corneal stromal surface under a flap during LASIK for one group of patients. The other group was not blotted at all. Results indicate corneal hydration levels affect the efficiency of laser ablation in LASIK procedures. Ablation effects were greater in patients with less hydrated corneas, but these patients underwent greater myopic progression.2
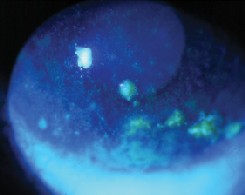
Staining reveals severe punctate keratitis in a post-LASIK patient. Courtesy: John Gingrich, O.D.
Another study published last August in the Archives of Ophthalmology evaluated the visual outcome, dry eye status and compli- cations of 543 eyes that underwent LASIK. The authors concluded that preexisting dry eye is a risk factor for severe postoperative dry eye with lower tear function, more vital staining of the ocular surface and more severe dry eye symptoms.3
Any patient demonstrating even a trace amount of SPK should be evaluated before undergoing LASIK. Try to discourage those with persistent SPK, significant exposure or Sjgrens syndrome from having the procedure. These patients may be candidates for refractive procedures available in coming years, but they are certainly predisposed to failure with LASIK, Dr. Phillips says.
Dr. Phillips also recommends a nasal flap for patients with mild to moderate dry eye who undergo LASIK. In order to make superior flaps, both nasal and temporal nasociliary innervation is severed, reducing sensitivity and setting up a complex dry eye management problem, he says.
Without doubt, the best approach is in patient selectivity, says Dr. Phillips, It is easier to manage preoperatively than postoperatively.
1. Goto T, Zheng X, Klyce SD, et al. Evaluation of the tear film stability after laser in situ keratomileusis using the tear film stability analysis system. Am J Ophthalmol 2004 Jan;137(1):116-20.
2. Kim WS, Jo JM. Corneal hydration affects ablation during laser in situ keratomileusis surgery. Cornea 2001 May;20(4):394-7.
3. Toda I, Asano-Kato N, Hori-Komai Y, Tsubota K. Laser-assisted in situ keratomileusis for patients with dry eye. Arch Ophthalmol 2002 Aug;120(8):1024-8.

