 |
The occurrence of an acquired brain injury (ABI) can be life-altering. The damage can be mental, emotional, cognitive and, of course, physical. The visual system can be impacted in a number of ways, including difficulty with eye teaming, focusing and tracking, double vision, visual information processing and visual field loss. According to a meta-analysis of 22 eligible publications, three visual conditions were identified as being commonly associated with traumatic brain injury (TBI).1 Random-effects models yielded the following combined prevalence estimates: accommodative dysfunction (42.8%), convergence insufficiency (36.3%) and visual field loss (18.2%). Another study reported many other visual dysfunctions associated with ABI, including loss of color discrimination, brightness detection and contrast sensitivity, visuospatial attention deficits with a slower response to visual cues, nystagmus, reading problems, saccadic and pursuit disorders and photosensitivity.2
In other columns, we’ve covered the topics of photosensitivity and double vision, but it is time to address the issue of visual field testing in patients suffering from ABI or TBI. As we all learned in optometry school, and perhaps in CE lectures, there are numerous methods for assessing visual fields, including confrontation fields, tangent screening, static perimetry (e.g., the Humphrey visual field by Zeiss) and kinetic perimetry (e.g., the Goldmann visual field).
The Goldmann is the gold-standard kinetic perimeter, since it establishes peripheral and central defects and correlates better than other options with activities of daily living.3 Unfortunately, in addition to the fact that the Goldmann equipment takes up significant real estate in the office due to its size, it requires a skilled technician to perform. It doesn’t help that the devices are no longer being manufactured. The Octopus 900 by Haag-Streit, an alternative kinetic perimeter, also provides a full 90° field, but it is automated. The advantage here is an improvement in test-retest reliability and a decrease in testing time. A study of 26 eyes from a neuro-ophthalmology clinic comparing the Goldmann with the Octopus found that 88.5% of subjects were correctly matched for normal or abnormal visual fields, and 89% of quadrants matched between the two tests.4
The same study found that 88.5% of subjects were correctly matched for normal or abnormal visual fields between the Octopus and the Humphrey static perimeter. A total of 80% of quadrants matched between these two tests. Despite the seemingly positive correlation in the results, we have not seen the same findings personally. We include one of our own cases highlighting the use of two systems in a brain-injured patient to demonstrate why we prefer the kinetic (Octopus) over the static (Humphrey) visual field.
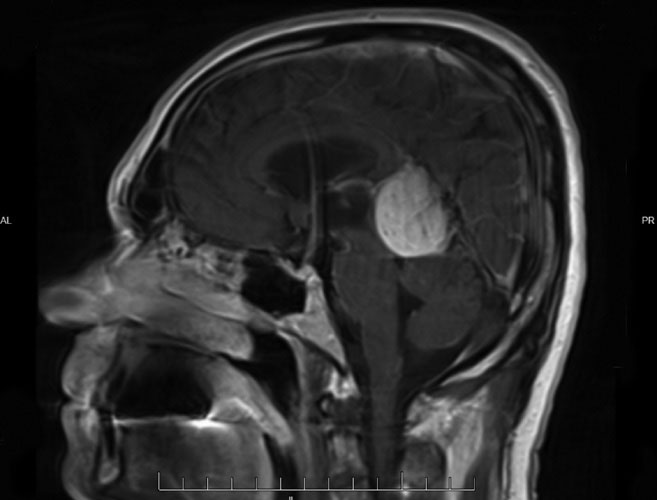 |
Falcotentorial meningioma near the pineal region. Click image to enlarge. |
Case Report
A 63-year-old white male presented to the Advanced Care Ocular Disease Service at SCO post-surgery for a left occipital craniotomy due to a falcotentorial meningioma near the pineal region two months prior. Immediately following the surgery, the patient complained of right-sided visual field loss, which had mostly returned by the time of the examination. He was concerned about driving again and was instructed to get an evaluation by his neurosurgeon. He was taking only two medications (allopurinol and bupropion HCl) and was otherwise healthy. His visual acuity was 20/20 OD, OS and OU, and his pupils were equal, round and reactive to light with no APD. Confrontation fields showed mild constriction on the right side OU. Out of caution, OCTs of the macula and optic nerve were completed and found to be normal. A 24-2 SITA Fast visual field showed a right homonymous hemianopsia that was denser superiorly, with macular sparing inferiorly, but not absolute. One thing to note was that the fixation losses OD and OS were quite high. The patient was counseled on the field loss and educated on and referred for vision therapy.
He reported several weeks later to the Vision Therapy and Rehabilitation Service with the same complaints as in the previous exam, with no improvement. The patient did not complain of diplopia, trouble with bumping into things on the right side or issues with balance. The chair skills were the same, including acuity and pupils. The fields by confrontation showed only right-sided constriction. A kinetic field on the Octopus using a III 4e target at 5°/sec showed slight constriction on the right side in both eyes: approximately 10% and 15% constricted in the right and left eyes, respectively.
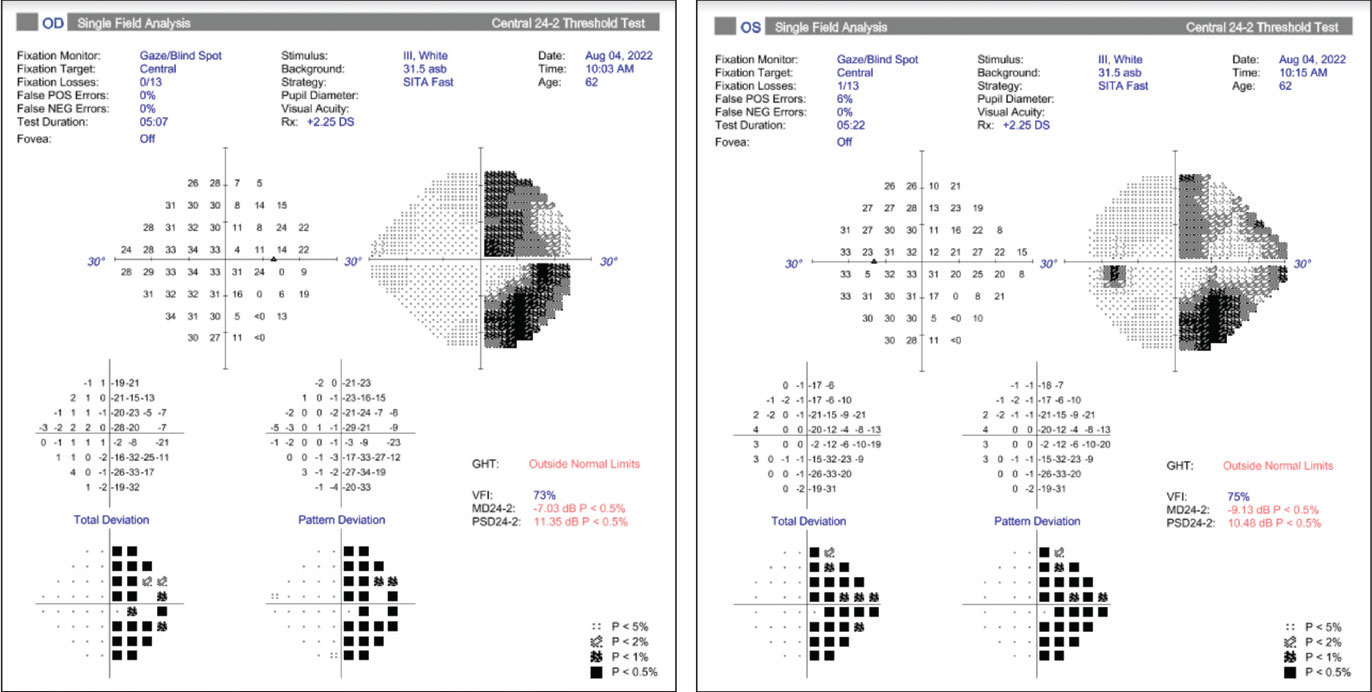 |
24-2 Humphrey visual fields showing non-absolute, right homonymous hemianopsia, denser superiorly with macular sparing inferiorly. Click image to enlarge. |
Based on the kinetic visual field and the patient’s minimal complaints, it was determined that vision therapy would be the best treatment option to assist him in learning some basic scanning concepts into far-right gaze, as well as to improve his visual attention to that side. Keep in mind that his ultimate goal was to get back behind the wheel. The plan was for the patient to complete 10 vision therapy sessions and then reassess his readiness for a driving evaluation by a specialized occupational therapist.
The therapy focused on peripheral attention and awareness and incorporated both free-space and computer-based activities. As with any therapy activity, feedback is crucial. The patient must know how they are performing so they can make adjustments and learn. Any opportunity to employ the other senses, particularly auditory and tactile, will assist the patient in creating new neurological pathways.
After 10 sessions, the patient’s kinetic field showed slight improvement, and he was asymptomatic. He was referred for driving evaluation and was thrilled when he passed with flying colors.
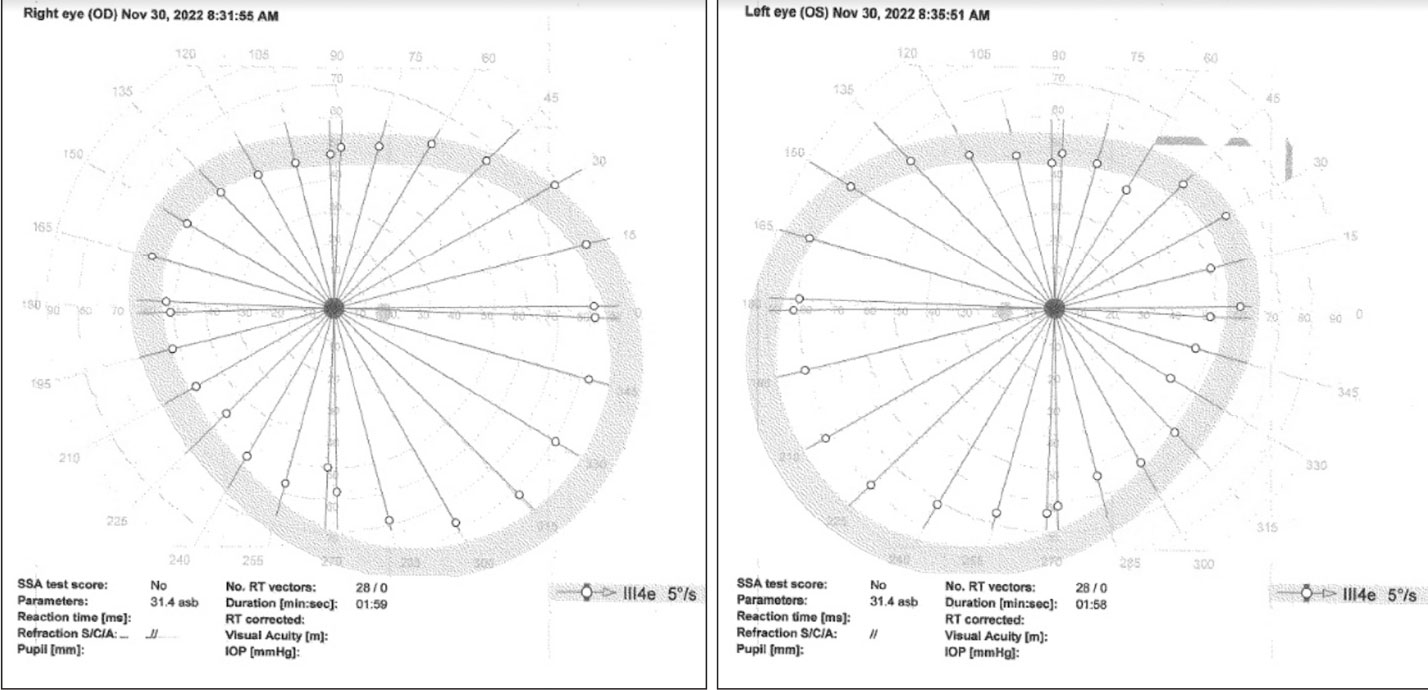 |
Octopus kinetic visual field using a III 4e target at 5°/sec showing only slight constriction. Click image to enlarge. |
Discussion
In this case, the two types of visual fields, kinetic and static, produced very different results. Even though there were several weeks between the tests, it is unlikely that the homonymous hemianopsia detected on the static visual field test dissipated that quickly. The two tests are quite different. The kinetic field measures 180° (technically 150° due to physical/physiological limitations), while the static field measures only 24°. The kinetic field has a constant target size and illumination, while the static field presents the illumination at different intensities to find the level of detection. The static field flashes the target for 0.2 seconds, while the kinetic target is constant. For patients who have trouble with attention and perhaps poor ocular motility, the quick flash of the target can be problematic and can potentially lead to poorer results.
Over our careers, we have seen countless patients who perform quite differently on the two visual field types. When evaluating brain injury patients, including those with neurologic disease, we have found that the kinetic field is more faithful to the true defect and provides a better understanding of the defect, especially in the periphery. For this reason, we recommend that practitioners who see a significant number of ABI or TBI patients in their offices consider using this valuable tool for a better visual field assessment
Dr. Taub is a professor, chief of the Vision Therapy and Rehabilitation service and co-supervisor of the Vision Therapy and Pediatrics residency at Southern College of Optometry (SCO) in Memphis. He specializes in vision therapy, pediatrics and brain injury. Dr. Schnell is an associate professor at SCO and teaches courses on ocular motility and vision therapy. She works in the pediatric and vision therapy clinics and is co-supervisor of the Vision Therapy and Pediatrics residency. Her clinical interests include infant and toddler eye care, vision therapy, visual development and the treatment and management of special populations. They have no financial interests to disclose.
1. Merezhinskaya N, Mallia RK, Park D, et al. Visual deficits and dysfunctions associated with traumatic brain injury: a systematic review and meta-analysis. Optom Vis Sci. 2019;96(8):542-55. 2. Singman EL. Automating the assessment of visual dysfunction after traumatic brain injury. Med Instrum. 2013. 3. Grobbel J, Dietzsch J, Johnson CA, et al. Normal values for visual field, corrected for age and reaction time, using semiautomated kinetic testing on the Octopus 900 perimeter. Transl Vis Sci Technol. 2016;5:5. 4. Bhaskaran K, Phuljhele S, Kumae P, et al. Comparative evaluation of Octopus semi-automated kinetic perimeter with Humphrey and Goldmann perimeters in neuro-ophthalmic disorders. Indian J Ophthalmol. 2021;69(4):918-22. |

