 |
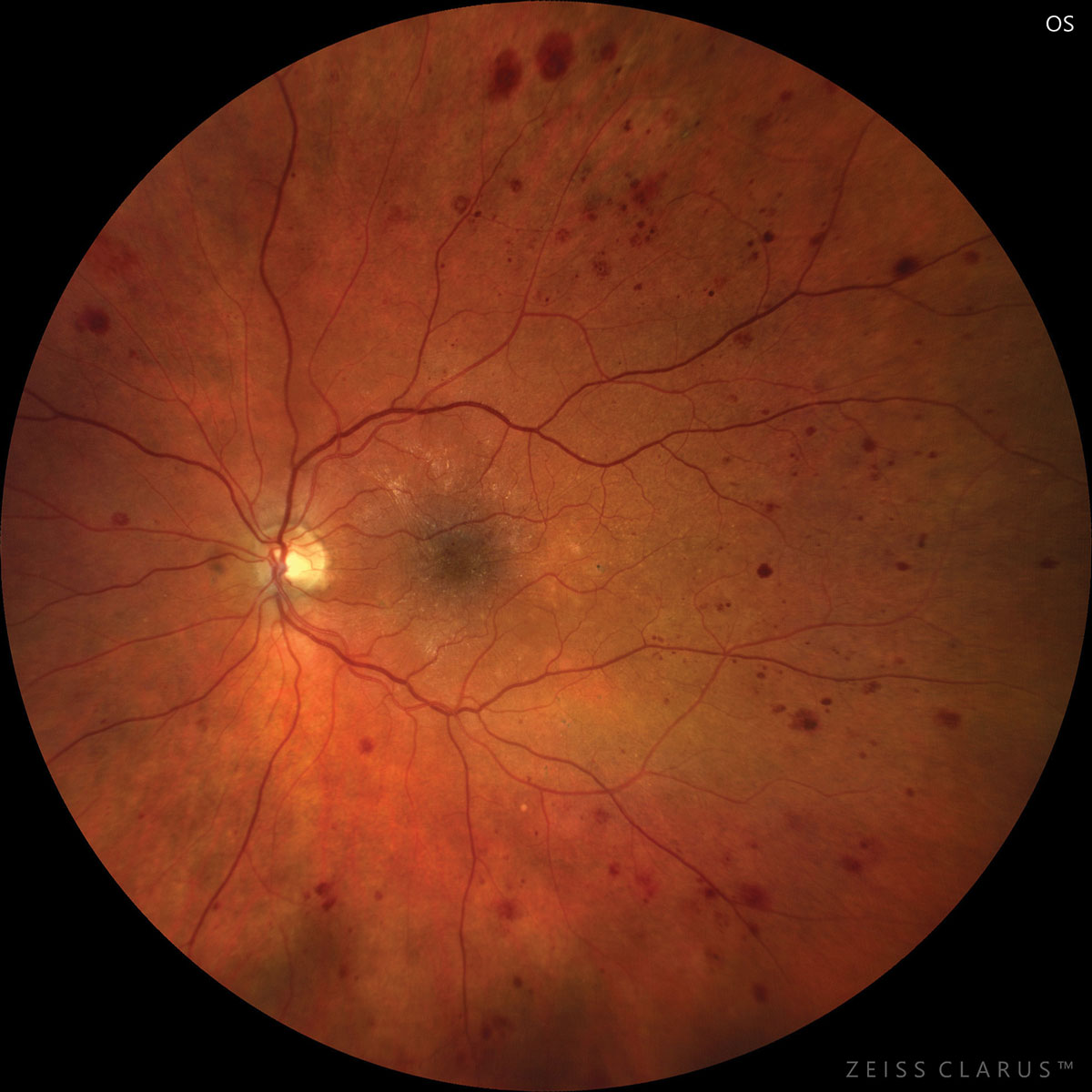
| Diabetic retinopathy represents an independent risk factor for stroke, suggesting microvascular pathology plays a role. Photo: Jay Haynie, OD. Click image to enlarge. |
A recent study followed patients with diabetes to determine the prevalence of disease affecting blood flow in the brain. Two centers, in Milan and Belfast, enrolled a total of 516 eyes from 258 diabetic patients. Ultra-widefield color fundus photography was graded for diabetic retinopathy severity and predominant peripheral lesion presence (>50% of the lesion). OCT-A was obtained in 252 eyes, which was examined for perimeter, area and circularity of the foveal avascular zone and vessel density, perfusion density, fractal dimension on superficial, intermediate and deep capillary plexuses and flow voids in the choriocapillaris.
Of the 516 eyes, 20.9% had no diabetic retinopathy. Another 10.3% had mild nonproliferative retinopathy, 38.2% had moderate nonproliferative retinopathy, 11.8% had severe retinopathy and 17.6% had proliferative retinopathy.
The study researchers found that worse retinopathy stage was associated with a history of stroke. After analysis taking into account factors of sex, type of diabetes, duration of disease and OCT-A variables, perfusion density and vessel density of the intermediate capillary plexus were found to be associated with stroke presence and retinopathy severity.
The authors pointed to prior studies finding similar results, with one concluding that those with type 2 diabetes and moderate nonproliferative retinopathy or worse at baseline have greater than a two-fold increased risk of subsequent stroke compared with mild or no retinopathy.
Their findings that perfusion density and intermediate plexus vessel density were associated with stroke may be indicative that diabetic patients with history of stroke have sustained large modifications to the retinal microcirculation. As the researchers explain, retinal vascular lesions likely reflect similar pathological processes in cerebral microcirculation due to the retina and brain sharing similar embryological origin, anatomic and physiologic traits.
The link between perfusion density and intermediate plexus vessel density with stroke strengthens the hypothesis that there is an existing association between retinal damage and damage to the cerebral circulation in diabetic patients.
Further, they wrote in their paper that “the results demonstrate the presence of association between OCT-A quantitative metrics and a history of stroke, highlighting that specific OCT-A parameters could be helpful in identifying a subgroup of patients with higher risk of cerebrovascular events. Future studies characterizing the type of stroke with strict control of other risk factors could be helpful in defining more in detail the nature of the association.”
The authors concluded that OCT-A could predict only about 32% of retinopathy severity evaluated on ultra-widefield imaging. They propose that “this may suggest that macular and peripheral modifications in diabetic retinopathy may be independent to a certain level and that both ultra-widefield imaging and OCT-A may be necessary for better understanding of retinal microvascular modifications due to diabetes.”
Vujosevic S, Fantaguzzi F, Salongcay RP, et al. Multimodal retinal imaging in patients with diabetes mellitus and association with cerebrovascular disease. Ophthalmic Res. May 30, 2023. [Epub ahead of print]. |

