 |
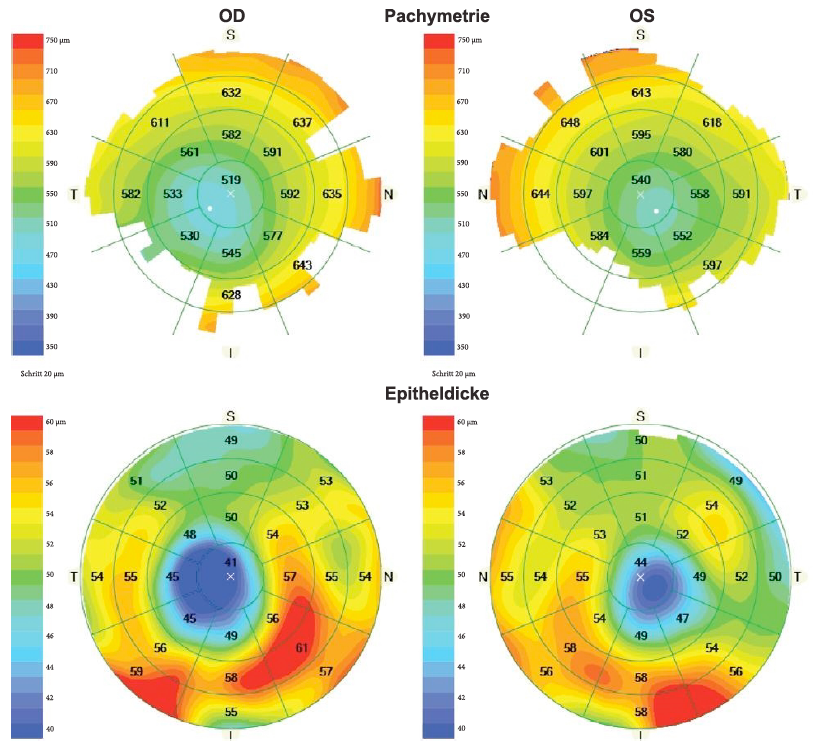
| This image from the study shows corneal and epithelial thickness maps of a patient with bilateral manifest keratoconus. Photo: Yucekul B, et. al. J Ophthalmol. May 25, 2024. Click image to enlarge. |
The clinical features of keratoconus differ greatly between adults and children due to relative lack of symptoms in children, making an early diagnosis difficult. Reliable clinical tests are especially important in this population, so, in a new study, researchers assessed the applicability of an algorithm developed for keratoconus detection in adolescents that relies on corneal pachymetric and epithelial thickness alterations derived from anterior segment OCT.
A total of 19 pediatric patients under the age of 18 diagnosed with keratoconus were included, and were divided into four groups according to the Belin-Ambrosio display (Pentacam): normal, manifest keratoconus, subclinical keratoconus, asymmetric eye with normal topography and tomography. Of these, 29 were manifest keratoconic eyes, three had subclinical keratoconus and five had asymmetric findings. In addition, 22 eyes from 11 normal adolescents were included.
Corneal and epithelial thickness maps were evaluated by a human grader. In the first step, if at least one of four pachymetry parameters (minimum, minimum-median, superonasal-inferotemporal and epithelial) exceeded its cut-off value, the eye was considered as suspect. In the second step, the combined presence of coincident thinning of total cornea and epithelium as well as concentric epithelial thinning lead to the diagnosis of keratoconus. Values for area under the curve, sensitivity and specificity were calculated.
Epithelial thickness assessments may increase the sensitivity and specificity of keratoconus screening compared to corneal topography alone and may be useful in diagnosing keratoconus in clinical practice, the researchers noted in the paper on their study, recently published in Journal of Ophthalmology. Such epithelial thickness changes in keratoconus have been studied by other authors with different devices in adults.
“In one of these studies, central corneal thickness, stromal layer thickness and central epithelial thickness were significantly different in eyes of adult keratoconus patients from the control group. However, in the pediatric population, epithelial thickness maps have only been examined in healthy children with AS-OCT,” the authors wrote. “In this study, epithelial thickness map characteristics of pediatric patients belonging to different stages of keratoconus were evaluated for the first time.”
The minimum-median and superonasal-inferotemproal pachymetry results showed statistically significant differences in manifest and subclinical keratoconus groups compared with the control group. These two measures showed the highest area under the curve results of the four, the authors explained.
In step two of the decision algorithm, coincident thinning and epithelial concentric thinning were seen in 100% of the manifest and subclinical keratoconic eyes of children. A previous study (Yang et. al) showed coincident and epithelial concentric thinning together in 97.8% of manifest keratoconic and 100% of subclinical keratoconic eyes of adults.
The researchers conclude by offering that using OCT and Scheimpflug imaging modalities together may improve the diagnostic accuracy of keratoconus in the pediatric population.
Yucekul B, Forster A, Burkhard Dick H, Taneri S. Detecting keratoconus in adolescents with anterior segment optical coherence tomography. J Ophthalmol. May 25, 2024. [Epub ahead of print.] |

