 |
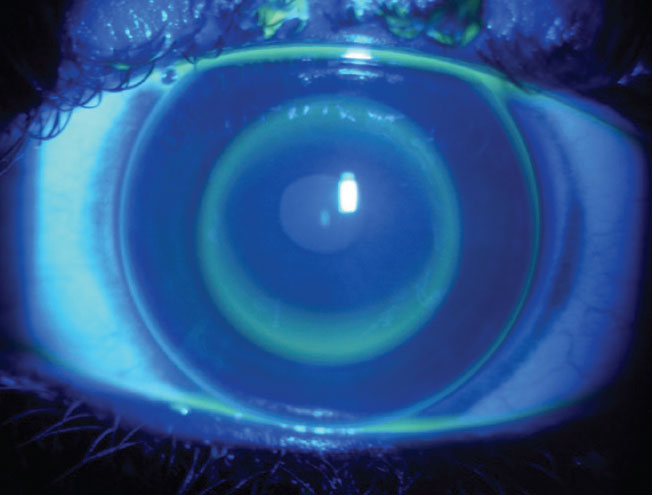
| Ortho-K wearers who already have evidence of corneal staining should see improvements in symptoms before any refractive surgery, as about 20% to 55% of patients report persistent dry eye symptoms after surgery. Photo: Kevin Chan, OD, MS, and Steven Sorkin, OD. Click image to enlarge. |
Orthokeratology (ortho-K) is a great option for many patients’ varying ocular needs; however, the modality may cause some issues when users want to transition to something different. Refractive surgery is a possibility with this patient population, but a prior history of ortho-K may impose constraints. In a new meta-analysis appearing in Eye & Contact Lens, researchers conducted a literature review to seek what parameters have changed after lens discontinuation, paying attention to which ones may affect refractive surgery.
A total of 41 articles described various ocular changes associated with ortho-K use. These included higher corneal staining, central corneal epithelial thinning and midperipheral thickening, increased higher-order aberrations, decreased contrast sensitivity, reduced corneal hysteresis and corneal resistance factor and tear proteome alterations. Positively, most of these parameters returned to baseline after discontinuation of ortho-K, but the timing in which this occurred may be dependent on the amount of myopic correction, ortho-K duration and age of lens fitting.
The authors of the study convey in their paper that mechanical pressure created by ortho-K on central epithelial cells can redistribute the epithelium from the center to midperiphery, thus inducing patterns of central corneal epithelial thinning and midperipheral thickening. These changes could be an issue with LASIK, since the epithelium/stroma ratio will vary across a 110µm flap created via femtosecond laser. This could affect flap integrity, increase risk of striae formation and decrease central residual stromal bed, which could lead to unpredictable ablation treatment and an increased risk of post-op ectasia.
Another worry is that ortho-K can possibly trigger stromal keratocyte apoptosis, worsening the potential for postoperative stromal haze formation to occur due to increased keratocyte activation. Apoptosis would lead to activating the wound healing response and subsequently keratocyte activation; thus, clinicians should be aware that this patient population may have an elevated risk of haze formation after surgery.
Despite these as well as other risks, most physiologic changes returned to baseline after discontinuation of the lenses. Cellular epithelial changes recovered, but endothelial changes like polymegethism remained. Some patients’ refractive error did not recover after lens discontinuation, with a pattern seeming to form of lag in recovery for refractive correction compared with corneal thickness and curvature. As such, the authors recommend “clinicians perform multiple serial tomographic and refractive measurements after ortho-K discontinuation to monitor the return to baseline and stability of these parameters before recommending corneal refractive surgery.”
The authors also write about factors that may influence the amount of time needed for lens discontinuation, including myopic refractive correction, total lens wear duration and age at which treatment is discontinued. They continue to outline that the stability needed to consider refractive surgery can be defined as the normalization of the keratometry of the anterior surface, regularization of the corneal surface and consistency of the patient’s refraction.
| Click here for journal source. |
Wang VM, Moin KA, Hoopes PC, Moshirfar M. Corneal refractive surgery considerations in patients with history of orthokeratology. Eye Contact Lens. November 7, 2024. [Epub ahead of print]. |

