 |
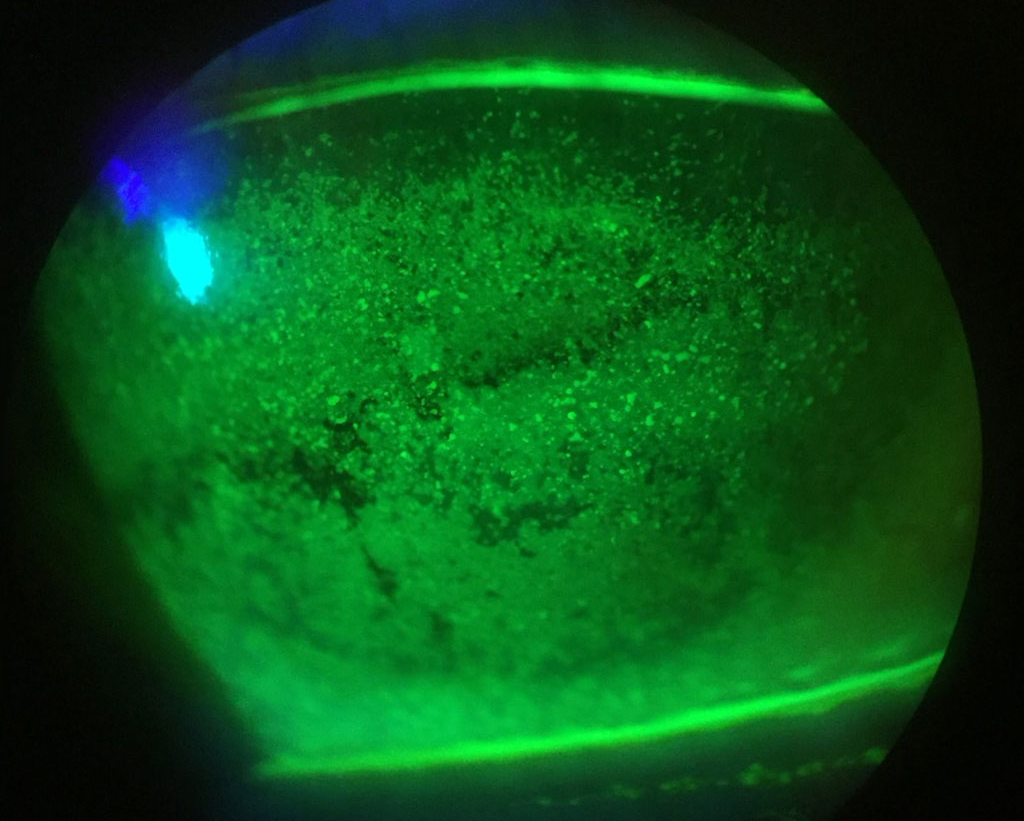
| The discordant phenotype of DED presenting with symptoms but no or minimal signs could reflect dysfunction of the central and/or peripheral somatosensory nociceptive pathways. Photo: Alexandra Wiechmann, OD. Click image to enlarge. |
One recent meta-analysis conducted by researchers examined multiple studies across databases to review the relationship between pain and dry eye. Specifically, researchers from Queensland University in Australia wanted to evaluate the relative contributions of objective and subjective indicators of dry eye disease (DED) in patients with chronic pain conditions vs. controls.
Included in the meta-analysis were 14 total observational studies encompassing 3,281,882 individuals. All included studies had the International Association for the Study of Pain International Classification of Disease (ICD)-11 codes for chronic pain conditions applied. Upon analysis, high quality evidence supported that those with chronic pain were more likely to experience DED symptoms than controls, with these symptoms being more severe with a clinically meaningful effect size. Chronic pain patients also displayed more rapid tear film disruption and reduced tear production compared with controls with moderate quality evidence. Those with chronic pain also had lower basal tear production (anesthetized) based on high quality evidence. However, tear film osmolarity did not display significant differences between the groups, and group differences for DED signs were not considered clinically meaningful.
In their discussion, the study authors elaborate that despite the group differences for DED signs being statistically significant, they were arguably of subclinical effect size, suggesting dry eye symptoms in those with chronic pain may not be fully attributable to ocular surface pathology. Indeed, this discordant phenotype of DED of symptomatology but with minimal or no signs may reflect central and/or peripheral somatosensory nociceptive pathway dysfunction.
What’s more, rapid tear film instability in irritable bowel syndrome was revealed upon subgroup analysis, as was a higher tear film osmolarity in fibromyalgia than for other chronic pain conditions. These were clinically meaningful but it should be noted that these instances may reflect inherent differences between various chronic pain conditions. Also clinically meaningful was the difference in DED symptoms for the Ocular Surface Disease Index between chronic pain patients and controls.
The increased prevalence and severity of DED symptoms in chronic pain conditions was not matched by clinical signs of the condition. Tear film osmolarity was not different between the groups and only a small, subclinical magnitude was observed with measures of tear break-up time and Schirmer Test 2. The only clinically significant one observed was a reduction in tear production (Schirmer Test 1).
Since these patients may be experiencing worse DED due to underlying nociceptive processing dysfunction or neuropathic mechanisms, the authors suggest that “highly symptomatic individuals with a chronic pain comorbidity may benefit from treatment targeting neuropathic and/or nociplastic mechanisms (such as a multimodal approach with initial use of anti-inflammatory agents and centrally acting medications including α2δ ligand anticonvulsants, tricyclic antidepressants and serotonin-norepinephrine reuptake inhibitors, or improving physical activity, sleep and stress, respectively)” and also encourage a knowledge of mental health associations and a multidisciplinary management approach.
They also add that “clinicians managing patients with a chronic pain condition should be cognizant of associations with symptomatic DED and refer to optometry/ophthalmology when indicated.”
Hoffmann M, Farrell S, Colorado LH, Edwards K. Discordant dry eye disease and chronic pain: a systematic review and meta-analysis. Cont Lens Anterior Eye. 2024:102248. |

