 |
Q:
Shingles has devastated the corneal sensation in one of my patients who has a persistent corneal defect from the resulting neurotrophic cornea. I’ve tried serum tears and amniotic membranes twice to no avail. How should I approach this?
A:
For the cornea specialist, neurotrophic keratopathy is one of the most challenging conditions to manage. Its chronic and relentless nature causes frustration among patients, who often try multiple different medications without seeing any significant improvements. Fortunately, our arsenal of tools to manage this disease has broadened significantly over the past five to 10 years, with newer tools demonstrating increasing promise.
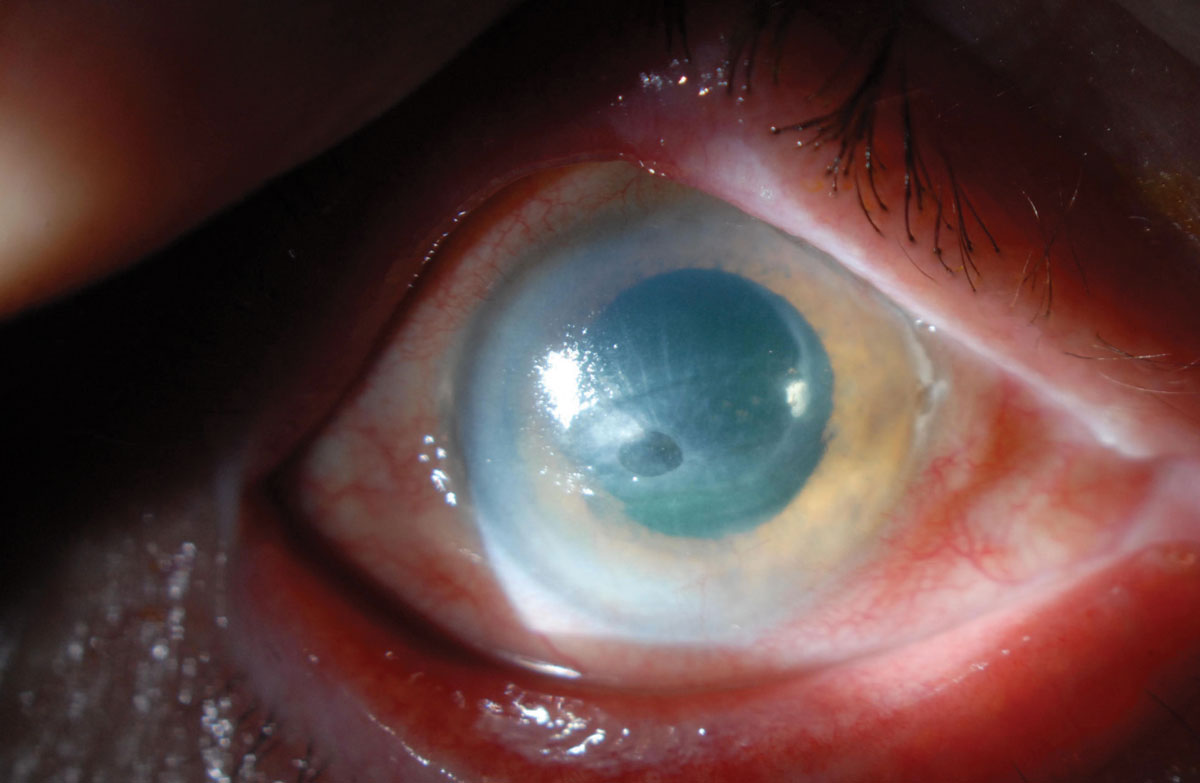 |
| A non-healing corneal ulcer in an eye with a history of herpes zoster ophthalmicus. Note the heaped-up epithelial edges. The radial striae indicate significant corneal thinning. Click to enlarge. |
Maneuvering Management
Neurotrophic keratopathy severity can be broadly classified into three stages.1 Stage one (mild) involves ocular surface irregularity, while stage two (moderate) presents with non-healing epithelial defects and stage three (severe) involves corneal ulceration with subepithelial tissue loss. Stage three is particularly concerning because of its potential to progress to corneal perforation.
While stage one disease can be treated with frequent lubrication (typically preservative-free artificial tears every two hours during the day), stages two and three often require more aggressive management. Punctal plugs, serum tears, bandage contact lenses, self-retained amniotic membranes and amniotic membrane transplantation are often used to promote healing. Referring patients to an oculoplastic surgeon for a temporary tarsorrhaphy—surgical closure of the eyelids over the corneal defect—often results in resolution of the defect. Christopher J. Rapuano, MD, chief of the cornea service at Wills Eye Hospital, recommends this course of action for this patient.
Another potential solution is referring patients to a contact lens specialist for a scleral lens fitting. By vaulting over the cornea, scleral lenses create a tear-filled space that keeps the ocular surface hydrated and protects the cornea from the microtrauma associated with blinking. Occasionally, serum tears are used with scleral lenses to bathe the cornea in the serum tears throughout the day. An additional benefit of a scleral lens includes refractive error correction.
Recently, interest has grown in the use of recombinant human nerve growth factor (rhNGF) agents to improve corneal health in patients with neurotrophic keratopathy. The REPARO trial evaluated the efficacy of rhNGF agents in promoting corneal epithelial healing in cases of moderate-to-severe neurotrophic keratopathy.2 Compared with vehicle-treated eyes, those treated with rhNGF agents achieved higher rates of healing at four and eight weeks.2 This effect appears to last for at least one year.
The commercially available rhNGF agent, Oxervate (cenegermin-bkbj, Dompé), entered the market in January of this year and should be administered six times a day for eight weeks. Common adverse effects of the drug are eye pain and hyperemia. In this patient’s case, Zeba A. Syed, MD, co-director of the cornea fellowship at Wills Eye Hospital, believes it is reasonable to start Oxervate now or after the epithelial defect has healed from the tarsorrhaphy.
Finally, in rare circumstances, we can look to our plastics colleagues to assist us in performing corneal neurotization procedures. This surgery provides an alternate source of innervation that serves to stabilize the corneal epithelium and help ensure success if a future keratoplasty is needed for corneal opacity secondary to neurotrophic keratopathy.
We can achieve corneal sensory reconstruction using one of several nerves, such as a branch of the sural nerve, with the supratrochlear nerve serving as the donor nerve. There is documented evidence of improved corneal sensation six to eight months post-procedure.3
These treatment regimens may be used in combination to rehabilitate the ocular surface, but ultimately deciding which management path to pursue depends on disease severity, prior treatment regimens, clinician experience and comfort level.
Although neurotrophic keratopathy is a difficult clinical condition to manage, the recent expansion of treatment options has enhanced our ability to achieve successful results.
| 1. Mackie IA. Neuroparalytic keratitis. In: Fraunfelder FT, Roy FH, Grove J, eds. Current Ocular Therapy. 4 ed. Philadelphia: WB Saunders;1995:452e454. 2. Bonini S, Lambiase A, Rama P, et al. Phase II randomized, double-masked, vehicle-controlled trial of recombinant human nerve growth factor for neurotrophic keratitis. Ophthalmology. 2018;125(9):1332-43. 3. Elbaz U, Bains R, Zuker RM, et al. Restoration of corneal sensation with regional nerve transfers and nerve grafts: a new approach to a difficult problem. JAMA Ophthalmol. 2014;132(11):1289-95. |

