 |
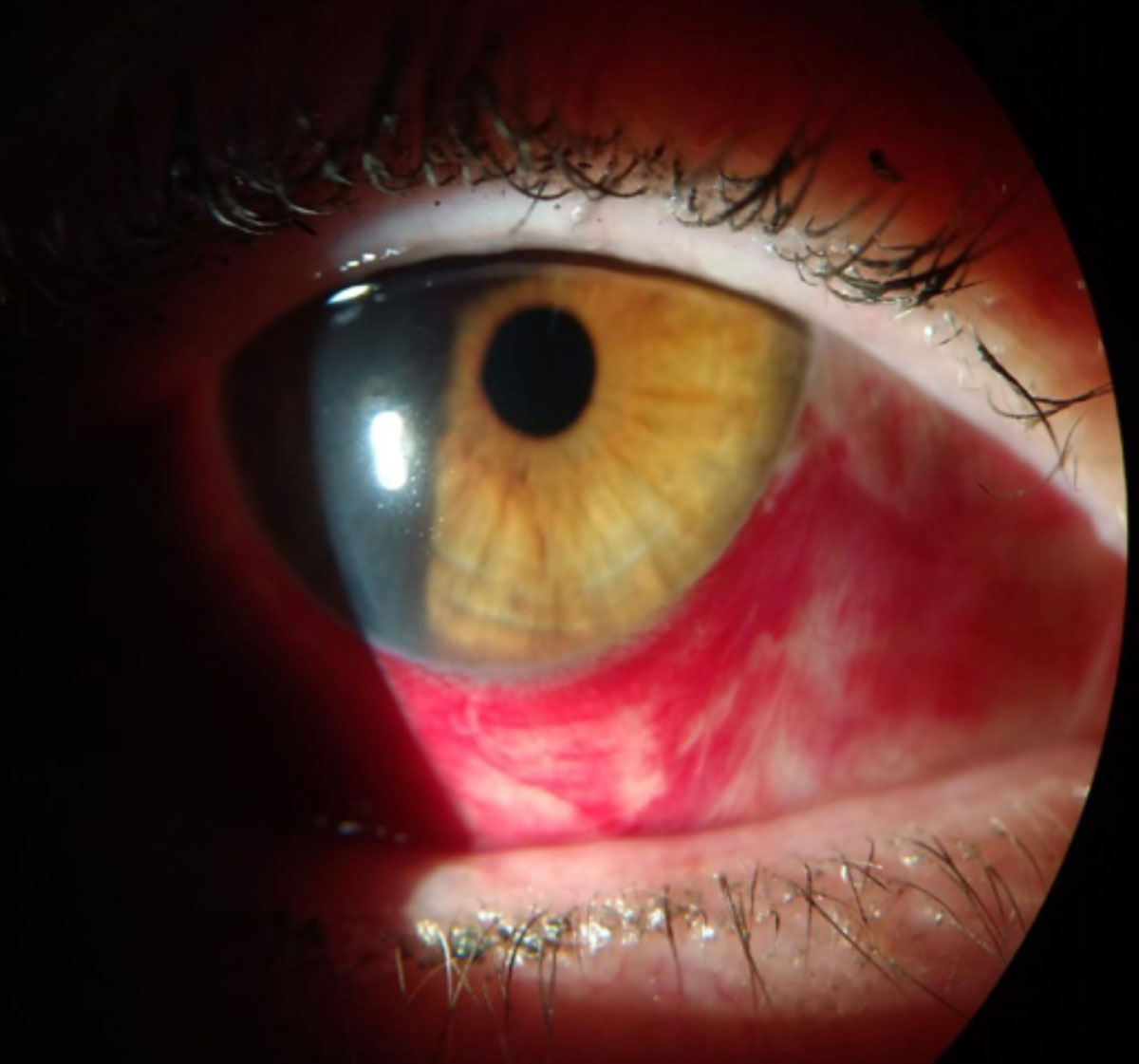
| Do surgeons have a duty to document relatively minor complications like subconjunctival hemorrhage (seen here in a nonsurgical patient)? Opinions differ. Photo: Julie A. Tyler, OD. Click image to enlarge. |
Certain cataract surgery complications, such as a posterior capsule tear requiring vitrectomy, are nearly universally agreed upon by surgeons as events requiring disclosure both in the operative report and to the patient. For non–visually threatening intraoperative complications (so-called “gray area” surgical complications) like subconjunctival hemorrhage and minor but troublesome concerns, there are no guidelines regarding appropriate documentation and/or patient disclosure. Perspectives and practice patterns may vary when such events occur, especially if a surgeon believes that a given condition is unlikely to cause serious long-term injury to the patient.
Researchers recently discovered that significant differences based on gender, practice setting and level of experience exist in regard to disclosure and documentation of these gray area complications from cataract surgery. Female surgeons were more likely than male surgeons to disclose them to their patients and experience psychological anxiety with regard to patient outcomes. Both early- and late-stage residents were more likely to believe that these conditions could lead to vision-limiting outcomes as compared with attending surgeons. Surgeons at academic centers were more likely than community-based surgeons to disclose the gray area complications in the operative report and experience psychological anxiety in regard to patient outcomes.
The researchers developed and distributed an anonymous online survey consisting of 11 potential intraoperative gray area surgical complication scenarios to practicing and resident ophthalmologists in the United States. Using a five-point Likert scale, participants assessed their perception of likelihood that a gray area surgical complication could lead to post-op complications, as well as their obligation toward patient disclosure and documentation in the operative report.
The study computed and averaged scores across (a) all 11 gray area surgical complication scenarios, (b) only ocular surface gray area scenarios and (c) only intraocular gray area scenarios. Scenarios involving corneal abrasion, chemosis and subconjunctival hemorrhage were considered ocular surface gray area surgical complication events. Scenarios involving Descemet’s membrane detachment, endothelial trauma, iridodialysis, iris prolapse, anterior capsule tear, posterior capsule tear, zonular dehiscence and damage to the intraocular lens were considered intraocular complication events.
Differences in Discretion
The study analyzed 389 responses. Overall, female surgeons were more likely than male surgeons to disclose gray area surgical complications (3.09 vs. 2.87). There was no gender difference in surgeons’ perspectives regarding the likelihood that these conditions would result in post-op complications or in disclosure in the operative report. For both ocular surface and intraocular complications, female surgeons were more likely than male surgeons to disclose them in the operative report (2.96 vs. 2.75; 3.19 vs. 2.88). There was no gender difference in surgeons’ concern that such events would result in post-op complications or in the likelihood of patient disclosure.
As level of experience increased among the four groups (early-stage resident, late-stage resident, early-career attending and late-career attending), surgeons were less likely to perceive postoperative complications from the gray area complications (2.60 vs. 2.38 vs. 2.21 vs. 2.19). For ocular surface complications, there was a positive correlation between level of experience and likelihood of patient disclosure. For intraocular complications, there was a negative correlation between level of experience and perceived likelihood of complications. No differences were seen in these four groups regarding the likelihood of patient disclosure or documentation. In general, resident surgeons were more likely to experience anxiety regarding patient outcomes.
Academic surgeons were more likely than community-based ones to disclose gray area surgical complications in the operative report (3.53 vs. 2.83). For ocular surface complications, community-based surgeons were more likely than those in academic settings to disclose them to their patients (3.03 vs. 2.66). However, for the same scenarios, academic surgeons were still more likely than community-based surgeons to disclose them in the operative report (2.97 vs. 2.35). No differences were noted in surgeons’ perspectives regarding the likelihood of perception that the conditions would result in post-op complications. For intraocular complications, academic surgeons were more likely than community-based surgeons to perceive postoperative complications from gray area complications (2.37 vs. 2.17), disclose them to their patients (3.16 vs. 2.83) and disclose them in the operative report (2.97 vs. 2.35). Overall, academic surgeons were more likely to experience anxiety regarding patient outcomes.
The researchers suggest factors such as departmental reporting requirements, supervising physicians’ scrutiny, concern for legal repercussions, fear of losing future surgical cases, apprehension regarding one’s surgical skills and potential loss of patients’ trust may cause specific surgeon demographics to be more likely to report and disclose gray area surgical complications.
“We emphasize that the purpose of our study was not to pass judgment or influence practice patterns regarding these conditions, but rather to inform our colleagues and bring awareness toward them,” the researchers wrote in their paper. “As this topic is a relatively new concept in ophthalmology, we hope that future studies can use our findings as a starting template and improve upon our limitations, including garnering a larger and more diverse number of respondents, enhancing training programs’ curricula and capturing perceptions toward these complications from international colleagues.”
Khan A, Murphy DA, Kloek CE, et al. Surgeons’ perspectives on intraoperative gray area surgical complications of cataract surgery. J Cataract Refract Surg. February 8, 2022. [Epub ahead of print]. |

